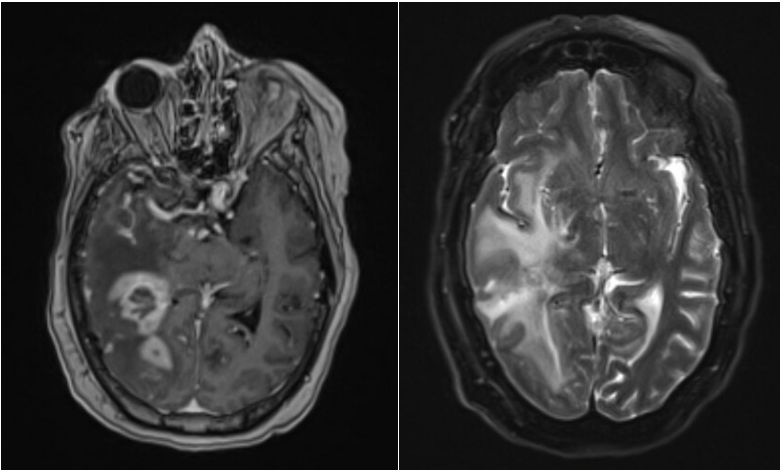
Case Presentation: A 58-year-old female presented to the hospital with fevers and L upper extremity weakness. She had a history of neurosarcoidosis diagnosed two years previously and treated with prednisone, infliximab, and mycophenolate mofetil. She had discharged ten days ago after a prolonged hospitalization for evaluation of multiple R cerebral lesions and mild leptomeningeal enhancement. In the initial hospitalization, a lumbar puncture (LP) showed elevated CSF protein (109mg/dL), 7 WBC/ul (81% lymphocytes), and negative studies including toxoplasmosis, cryptococcus, aerobic, fungal, and AFB culture. CSF cytological analysis and a brain biopsy were not obtained. Imaging of the chest and sinuses were unremarkable. She received treatment with vancomycin, ceftriaxone, and metronidazole, and she had completed 39 of a 42-day course. She previously received voriconazole which was stopped due to liver enzyme elevation. Upon the second hospital admission, she was febrile to 38.5C with tachycardia with exam showing 4/5 strength in the L upper extremity. Repeat MRI of the brain w/ contrast showed an increased size and number of peripherally enhancing lesions in the right hemisphere with associated vasogenic edema and peripheral restricted diffusion with a left midline shift (Figure 1). Blood cultures and CT imaging were unrevealing of etiology of fever. A LP was not performed due to midline shift. Brain biopsy, which occurred 6 days after the patient had started on IV dexamethasone, showed atypical, extensively necrotic lesion with mixed B- and T-cell infiltrate adjacent to necrotic CD20+ cells. Cultures of the mass including aerobic/anerobic, fungal, and AFB were negative. Rubidium PET scan showed known brain involvement but no systemic involvement. The patient transitioned to the oncology service for treatment of CNS lymphoma with R-MPV.
Discussion: The diagnosis of primary CNS lymphoma was delayed secondary to multiple confounding differentials including a history of neurosarcoidosis and concern for cerebral abscesses. However, there were aspects of this case that were atypical including the peripheral diffusion-restriction as abscesses usually have central diffusion-restriction1. The increase in size while on antibiotics raised concern for a malignancy. High dose dexamethasone and delayed biopsy decreased biopsy yield2. CNS lymphoma comprises about 2-3% of CNS malignancies3-4. Risk factors include immunosuppression, although most cases occur in elderly, immunocompetent patients2. While most cases are solitary, multiple lesions occur in 30% of cases, and up to 50% of cases in immunocompromised patients2,5,6. Immunocompromised patients are more likely to present with ring-enhancing lesions and necrosis6. Sarcoidosis-lymphoma syndrome was described in 19867. Patients with sarcoidosis develop lymphoproliferative disorders at an increased incidence7-8. There are few reports of sarcoidosis and development CNS lymphoma, and we could find no prior cases of a patient with known neurosarcoidosis developing CNS lymphoma9-10.
Conclusions: In cases of diagnostic uncertainty with brain lesions, a biopsy is important to confirm the diagnosis. Corticosteroids decrease the yield of the biopsy in CNS lymphoma. It is important to maintain a broad differential and multi-disciplinary approach including involvement of the radiologist to help establish the differential diagnosis.