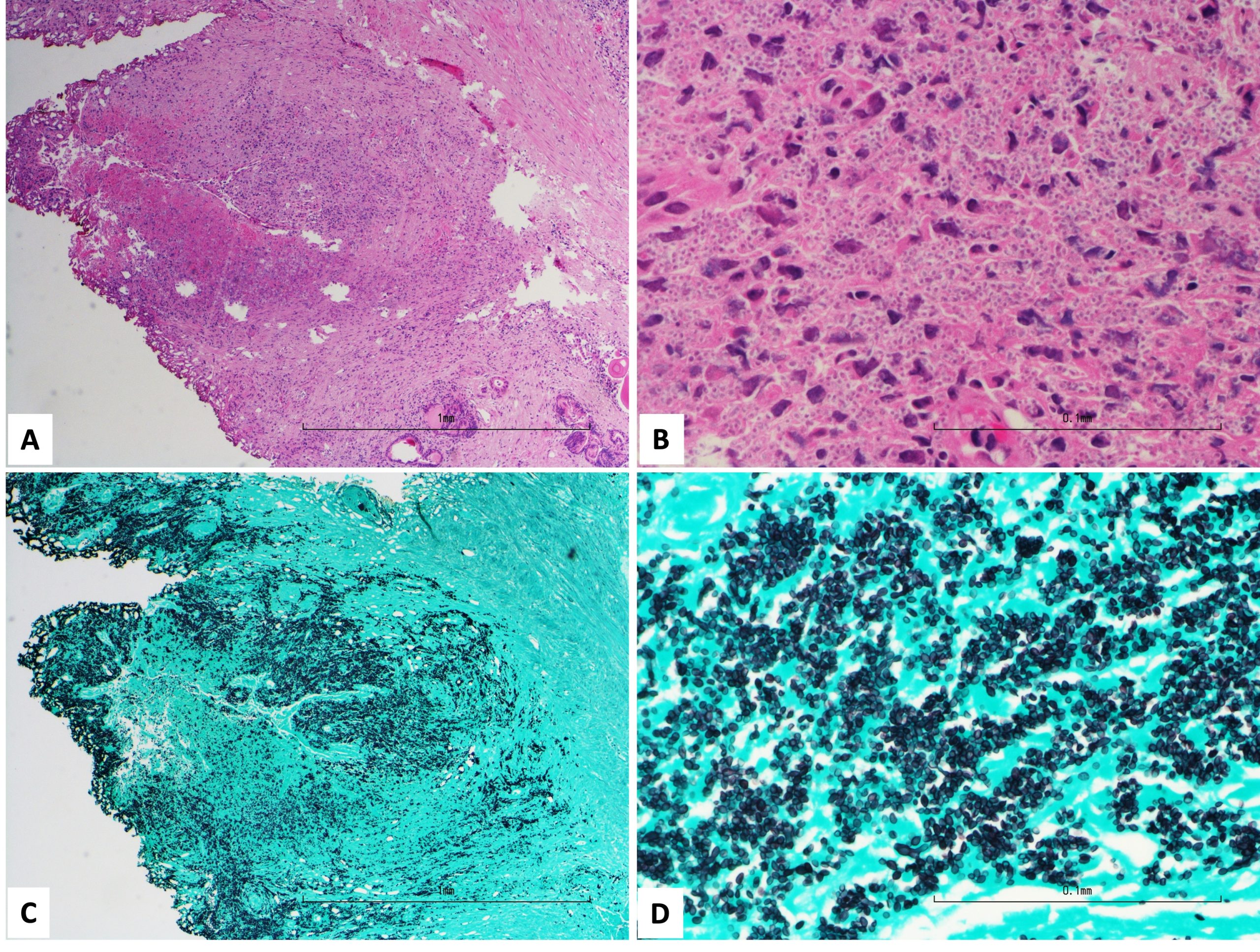
Case Presentation: A 54-year-old male with known human immunodeficiency virus (HIV) presented to the emergency room with three weeks of progressive lower abdominal pain, nausea, chills, and a 15-lb weight loss. The patient had no diarrhea, dysuria, urinary frequency, or penile discharge. He had no recent sexual activity. He was diagnosed with HIV four years prior to presentation and was not on antiretroviral therapy. Physical examination was notable for tachycardia, oral thrush, and enlarged, non-tender prostate on digital rectal exam. His HIV-1 RNA viral load was 331,000 copies/mL, and white blood cell count was 4,700/uL with neutrophilia (81.1%) and a CD4+ cell count of 39. CT scan of the abdomen found a 2.8 x 2.7 x 4.2 centimeter hypodense region in the right superior prostate. The patient was initiated on vancomycin, cefepime, and metronidazole to empirically treat prostatic abscess, but he had persistent fevers and myalgias. Urine cultures and blood cultures were without growth. He underwent transurethral resection of the prostate with minimal purulent drainage. Grocott methenamine silver stain of a prostate tissue sample revealed intracellular uniform budding yeast consistent with Histoplasma capsulatum. A Histoplasma urine antigen sent on admission subsequently returned positive. To evaluate for disseminated histoplasmosis, a CT chest was performed, which found only small bilateral centrilobular nodules. Following diagnosis, empiric antibacterials were stopped. The patient was started on IV amphotericin B and itraconazole, with rapid resolution of his fevers and symptoms. He was discharged with plan to continue itraconazole for one year.
Discussion: Histoplasma capsulatum is a dimorphic fungus endemic primarily to North and Central America.1-3 In the United States, Histoplasma was traditionally thought to be in the soil around the Ohio and Mississippi Rivers, but an increasing number of cases have been identified in much of the Eastern United States, with an estimated national annual incidence of 3 million infections.4 Histoplasmosis is known to spread hematogenously to other organs, particularly in immunocompromised patients. However, genitourinary involvement is exceedingly rare. Fewer than twelve cases of Histoplasma prostatitis have been reported in the literature and occurred primarily in patients with AIDS.5-13 More commonly reported mycoses with prostate involvement are blastomycosis and cryptococcosis, which also typically manifest in patients with impaired cellular immunity and can present with subacute, relatively nonspecific symptoms.14 In retrospect, our patient’s relatively nonspecific symptoms, persistent fevers despite broad-spectrum antibiotics, and minimal purulent drainage were diagnostic clues, even in the absence of clinical pulmonary findings. His immunocompromised status prompted initial testing for mycoses, mycobacterium, and other opportunistic infections, in addition to enteric and sexually transmitted bacteria more classically considered in patients admitted with prostatitis.
Conclusions: This case highlights the importance of considering fungi in prostatic infections, particularly in immunocompromised patients living in endemic regions. Genitourinary involvement of histoplasmosis is especially rare. Nonspecific symptoms and exam findings, as well as lack of improvement with broad-spectrum antibiotics, should raise suspicion for this rare disease and prompt additional testing.