Case Presentation: A 32-year-old female with anxiety and depression presented to the ED after seizure episode. Upon admission, the patient was hemodynamically stable with normal vital signs and laboratory analysis. Physical examination revealed an unresponsive, well-nourished female with her eyes closed, jaw clenched, and arms and legs rigidly extended, consistent with a dystonic episode. She received diphenhydramine which relaxed her jaw and extremities and ended the event. 20 minutes later, she experienced another event that was different in appearance from the previous episode and was terminated with the same medication, leading to the diagnosis of psychogenic non-epileptic seizures (PNES). Subsequent CT and MRI of the head were unremarkable. EEG was negative for any epileptiform discharges. Upon resolution of her symptoms, she denied a personal or family history of seizures, head trauma, or drug or other medication use. She revealed that two days ago while at talk therapy, she disclosed an episode of prior sexual abuse, which was emotionally painful. In the ensuing hours, she experienced intermittent eyelid twitching followed by shaking of the lower extremities. Over the next day, the leg shaking increased in intensity and spread to the arms, prompting her to seek medical attention. Over the course of her three-day hospitalization, she had multiple episodes, each one associated with a different rigid posture. These were captured on continuous video EEG and revealed no epileptiform discharges. Repeat laboratory testing was normal. She was diagnosed with PNES and was discharged home to be followed by psychiatry and neurology.
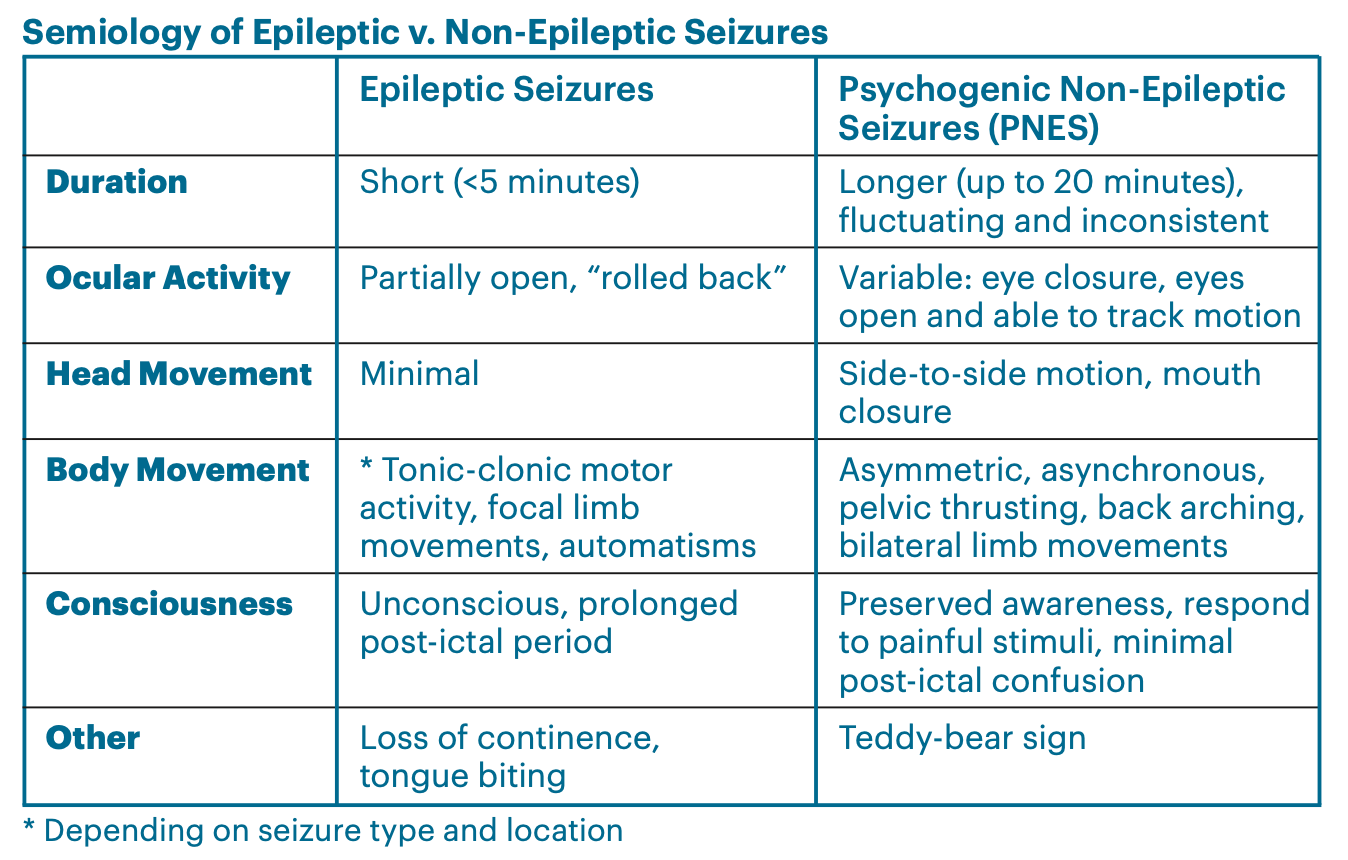
Discussion: The aim of the present report is to highlight the difficulties in formulating a differential diagnosis for PNES and discuss the psychiatric and neurological aspects of its treatment. PNES are seizure-like events characterized by behaviors, movements, sensations, or states of awareness that lack an organic, neurobiological pathology. PNES are thought to be somatic manifestations of underlying psychological unrest, and may resemble epileptic seizures, acute dystonia, or vasovagal syncope. Affected patients are at an increased risk of iatrogenic harm due to the difficulties in diagnosing and managing such seizures. Video EEG without epileptiform features as well as the semiology of non-epileptic seizures are used to support a PNES diagnosis. Once the diagnosis is made, treatment should focus on addressing psychiatric comorbidities and minimizing the use of anticonvulsants unless comorbid epilepsy is present.
Conclusions: PNES is a challenging diagnosis but should be considered in a patient with intractable seizures. It will guide future treatment options with the goal to decrease hospitalization and iatrogenic injury.