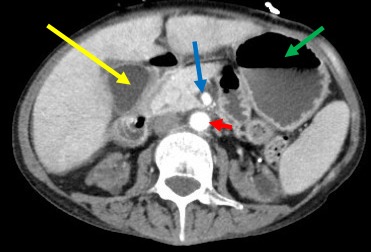
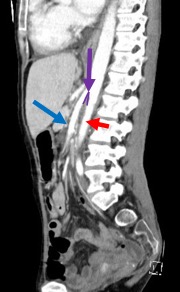
Case Presentation: A 33-year-old female presented to the emergency department with 2-days of fever, nausea, non-bilious/non-bloody vomiting, epigastric pain, and anorexia. This was superimposed on a one-year history of intermittent abdominal pain, bloating, nausea, bilious vomiting, and 20-pound weight loss which has been preceded by food insecurity with resulting weight loss. Her past medical, surgical, and social histories were otherwise non-contributory.On presentation, vital signs were normal. Physical exam revealed a cachectic female (BMI 13.45 kg/m2) with epigastric tenderness. Labs were significant for elevated lipase (1,030 U/L) and triglycerides (204 mg/dL). Computed tomography (CT) showed moderate gastric distention, and dilation of the proximal duodenum with a transition point at the third portion as it passed between aorta and superior mesenteric artery with narrowing of the aortomesenteric angle and no other significant findings.With conservative management, her pancreatitis improved. A gastrojejunostomy (GJ) stent was placed to facilitate weight gain through per oral means. She was discharged in improved condition with outpatient follow-up.
Discussion: Acute pancreatitis is defined as inflammation and auto-digestion of pancreatic tissue. Diagnosis requires at least two of three criteria: 1) epigastric pain; 2) amylase/lipase elevation (3x upper limit of normal); and/or 3) consistent imaging findings. Common causes include choledocholithiasis, alcohol use, hypertriglyceridemia, bacterial or viral infections, autoimmune disease, hypercalcemia, medications, anatomic pancreatic anomalies, and ischemia. SMA syndrome is a rare condition in which the loss of mesenteric fat between the SMA and the duodenum leads to a significant reduction in the angle formed by the proximal SMA and aorta (normally between 38 and 65 degrees), leading to compression of the third portion of the duodenum and proximal bowel obstruction. Symptoms include nausea, abdominal pain, bilious vomiting, and weight loss. Diagnosis is established by imaging with gastric distension, dilation of the proximal duodenum, reduced aortomesenteric angle, and a transition point at the third portion of the duodenum.This patient was diagnosed with acute pancreatitis from SMA syndrome, a very rare condition with only a few reported cases. Pathophysiology remains unclear, but proposed mechanisms are: 1) malnutrition causing pancreatic cell atrophy, dilatation of the ducts, and increased oxidative environment resulting in inflammation; 2) duodenal compression by the SMA causing secondary post-papillary syndrome and retrograde reflux of bile into the pancreatic duct and inflammation.Acute treatment often consists of gastroduodenal decompression, correction of electrolyte abnormalities, analgesia, fluid resuscitation, and nutritional support. Some patients can tolerate oral intake with dietary or behavioral modifications (such as small meals or pureed diet); however, some may require total parenteral nutrition. For persistent symptoms and oral intolerance, a GJ tube or stent may be placed for enteral nutrition. With weight gain and increased mesenteric fat, SMA syndrome can resolve, though some patients may require endoscopic versus surgical gastrojejunostomy or duodenojejunostomy to effectively bypass the obstruction.
Conclusions: It is important to consider SMA syndrome as a rare cause of acute pancreatitis, especially in patients presenting with symptoms / imaging consistent with this condition.