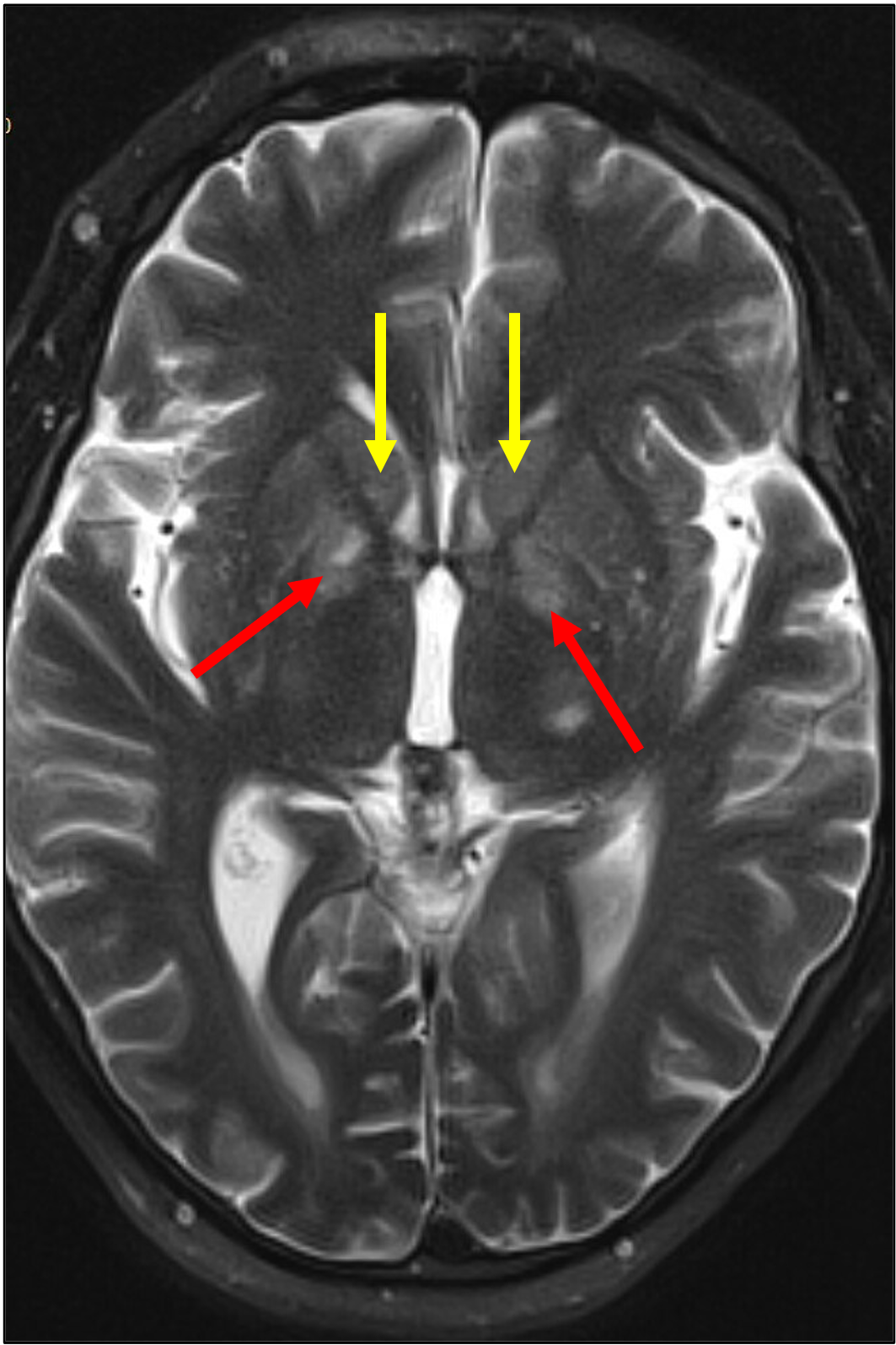
Case Presentation: A 51-year-old male with previous left-sided cerebellar ischemic stroke and NASH cirrhosis complicated by hepatic encephalopathy presented with 3 weeks of slowed speech, bradykinesia, abnormal facial movements (grimacing, lip smacking, tongue protrusion, and forced eye closure), and confusion. He denied alcohol or other drug use. On presentation, vitals were normal. He was oriented only to person and place. His speech was dysarthric and slow. His thoughts were tangential. He had a euphoric affect and protracted nonrhythmic, asymmetric, asynchronous facial movements and head nodding. He had no asterixis. Labs showed baseline anemia, thrombocytopenia, hypoalbuminemia, hyperbilirubinemia and mildly elevated aspartate and alanine transaminases, alkaline phosphatase, and INR. Serum ammonia, B12, folate, TSH, CBC, CMP, ethanol, copper, urinalysis, and urine toxicology screen were normal. Head CT showed left cerebellar encephalomalacia. Contrasted abdominal CT showed small portosystemic shunts.He was admitted and started on lactulose and rifaximin. Although his orientation improved, his neurologic changes persisted. Contrasted brain MRI showed abnormal T2/FLAIR signal in the bilateral caudate and globus pallidus regions (Figure 1). Serum ceruloplasmin, vitamin B1, manganese, and 24-hour urinary copper excretion were normal. He was diagnosed acquired hepatocerebral degeneration (AHD). He was discharged home on lactulose and rifaximin with referral for liver transplant evaluation.
Discussion: AHD is a rare disorder of abnormal movements and cognitive impairment caused by liver dysfunction, specifically chronic liver disease (CLD; prevalence of 1-2%).1 Risk factors include previous acute hepatic encephalopathy and the presence of portosystemic shunt(s).2,3 Pathophysiologic mechanisms are not clear. One theory proposes a combination of toxic substance accumulation (ammonia and manganese) in the brain and chronic systemic inflammation, leading to neuroinflammation, excitotoxicity, mitochondrial dysfunction, and neurodegeneration. Intracellular manganese accumulation in the basal ganglia results in neurotoxicity.4Neurologic signs and symptoms include: 1) movement disorder (parkinsonism, ataxia-plus syndrome)2,3; 2) cognitive impairment (disorientation, inattentiveness, psychomotor retardation, impaired memory/verbal fluency)5 and psychiatric symptoms (disinhibition, apathy, aggression, paranoia); and 3) myelopathy. Diagnosis is based on history, signs/symptoms, and characteristic findings on brain imaging including hyperintensity in the bilateral globus pallidus (parkinsonism) or high-signal lesions in the middle cerebellar peduncles (ataxia-plus syndrome).5,6 Serum manganese levels in AHD are variable, thus not diagnostic.7AHD symptoms may be managed with medications (e.g., levodopa for parkinsonism;8 dopamine receptor antagonists, tetrabenazine, anticholinergics for hyperkinetic movement disorders;9,10 rifaximin, and lactulose11). Obliteration of portosystemic shunts has shown occasional benefit.12 Liver transplantation may reverse both clinical and neuroradiologic findings in AHD.5
Conclusions: General internists should be familiar with acquired hepatocerebral degeneration as an uncommon cause of neurologic symptoms in chronic liver disease patients to avoid unnecessary diagnostics/therapeutics and prompt discussion about liver transplantation.