Background: Medication reconciliation (MR) is critical for patient safety during hospital admissions and transitions, though MR completion may be complicated by factors such as lack of familiarity with the electronic medical record (EHR) or missing information at admission. Over the past three years, our urban academic quaternary care hospital has led a successful MR improvement project on a General Medicine Teaching Service (GMTS). Using gamification and data sharing with resident physicians, we improved MR completion rates, but these strategies were time-intensive and their impact waned when no longer actively implemented. Here, we present the third phase of the project and propose next steps for sustaining improvements.
Purpose: This project aimed to improve MR completion by integrating electronic educational modules, gamification, dashboards, and worksheets to promote the use of the dedicated MR EHR tab and verification tool within the GMTS. The goal was to measure differences in MR tab use pre- and post-intervention, streamlining provider work and improving transitions of care for GMTS inpatients.
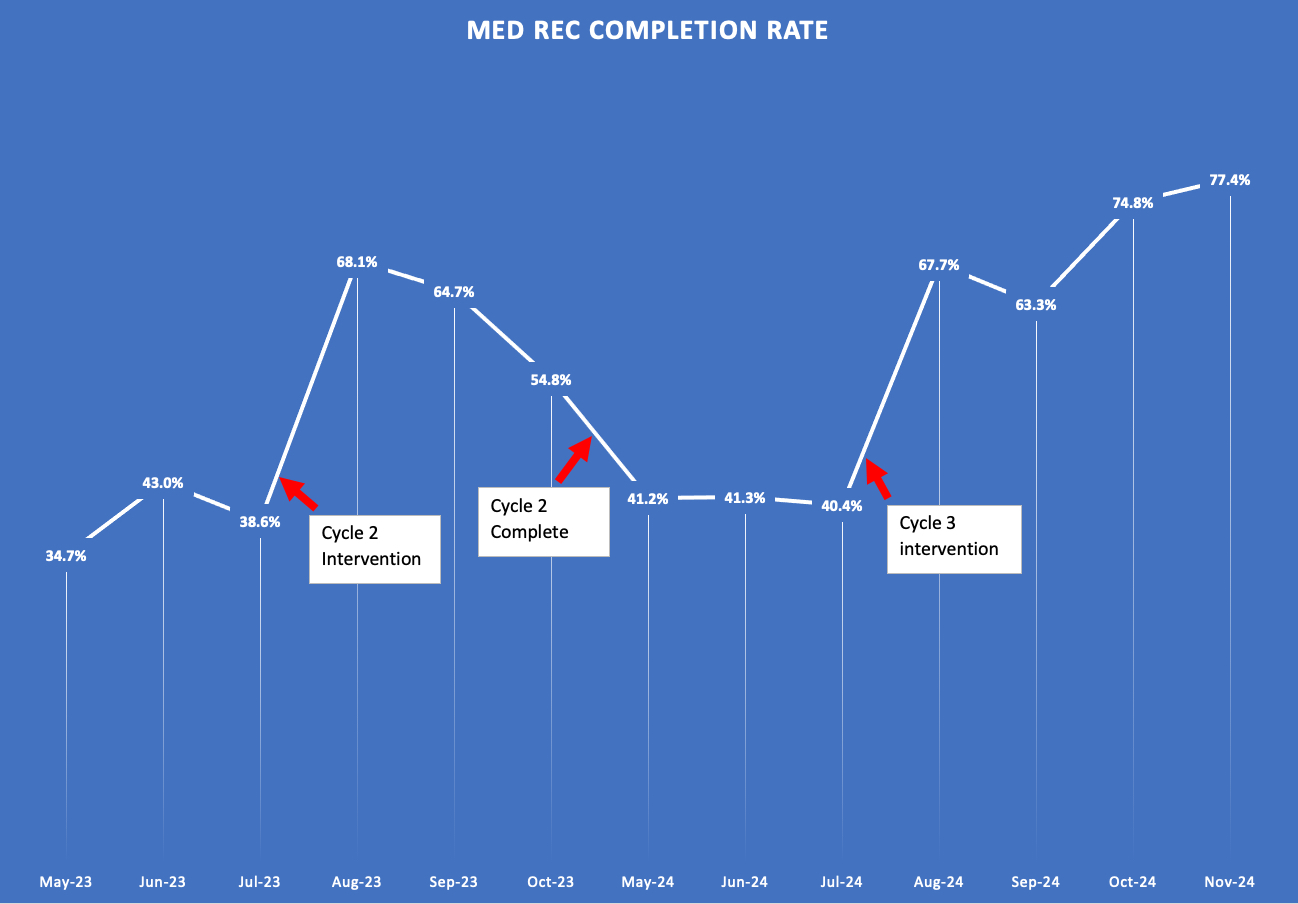
Description: A third PDSA cycle was conducted from July 29 to November 3, 2024. Previous interventions were continued, including onboarding incoming housestaff with workflows for MR completion, bi-weekly dissemination of workflows, in-person reviews, and weekly distribution of report cards to resident teams on MR completion rates. Gamification was reinstituted, with cookies awarded to teams achieving the highest completion rates at the end of each rotation.Three new interventions were introduced to ensure sustainability: first, dedicated time for MR completion, branded “Med Rec O’clock,” added to the resident daily schedule; second, MR worksheets were created and distributed to patients or caregivers to aid in MR completion; third, attending physicians were engaged by sending weekly MR dashboards to hospitalists on service.After the intervention period, a report of all admissions completed by residents on the GMTS was reviewed for MR completeness. MRs were counted as complete if the resident marked a designated drop-down menu as “Complete.” In the baseline period prior to the intervention, the average MR completion rate was 41.0%, which was slightly higher than the baseline of 38.8% in 2023 (χ2=1.1, p>0.25), and a large absolute increase from the pre-PDSA baseline of 22.9%. Over the 3-month course of PDSA cycle 3, the MR completion rate increased to an average of 67.8%, a statistically significant improvement from baseline (χ2=170.0, p< 0.01), and from the 62.4% rate observed after PDSA cycle 2 (χ2=6.23, p< 0.05). The highest completion rate of 77.4% occurred during the last block of the cycle. In total, 112 dashboards were distributed to 36 GMTS attendings. Survey data showed that only 20% of residents used the MR worksheets.
Conclusions: Over the past three years, gamification and education alone did not change the culture around MR completion. When these interventions were discontinued, MR completion rates remained higher than the previous baseline but significantly dropped afterward. Systematic changes are necessary to sustain these improvements. In this PDSA cycle, we introduced dedicated time for MR completion in the resident workflow and engaged attendings through data sharing. These process changes have resulted in improved MR completion rates, and we will continue to monitor the data to ensure sustainability.