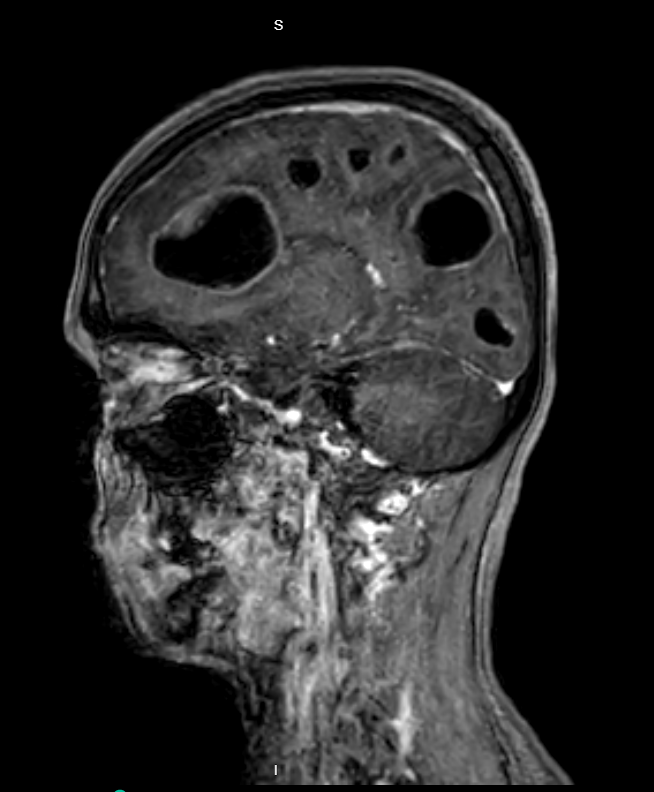
Case Presentation: A 40-year-old woman with a history of bipolar disorder and cannabis use disorder presented with four days of headache, dizziness, and vomiting. Initial examination revealed no focal neurological deficits except inconsistent orientation to time and cognitive slowing. She was treated symptomatically and planned for discharge. As she attempted to leave the ED, she was unable to ambulate due to unsteady gait.CT scan of the head and subsequent MRI showed multiple brain cysts, read as “suspicious for neurocysticercosis”. Dexamethasone and levetiracetam were started while antiparasitic treatment was deferred pending diagnostic confirmation and to reduce the risk of inflammatory complications. EEG was negative for seizure activity. Infectious work-up, including cysticercosis antibody, was negative. Chest x-ray showed no mass or infiltrate. By day three of hospitalization, the patient developed tangential speech, difficulty following commands, and worsened ataxia. CT scan of the chest revealed necrotic mediastinal lymph nodes. Endobronchial ultrasound (EBUS) showed an endobronchial lesion and multiple lymph nodes, which were biopsied. Histopathology confirmed small cell neuroendocrine carcinoma. The patient was diagnosed with small cell lung cancer (SCLC) with cystic brain metastases and subsequently received whole brain radiation and chemotherapy with etoposide/carboplatin.
Discussion: A patient’s psychiatric history and substance use can lead clinicians to minimize and misattribute neurologic symptoms. Diagnostic biases likely contributed to the initial underappreciation of her symptoms. The absence of focal findings on initial cursory examination led providers to suspect that her symptoms had no organic basis. Subsequently, the radiologist’s reading led to anchoring on neurocysticercosis as the cause of her imaging findings, and confirmation bias led to prioritization of serologies rather than evaluating for other etiologies with further imaging like chest CT. Fortunately, the patient was seronegative for cysticercosis, and the diagnostic evaluation was widened. SCLC accounts for approximately 15% of all lung cancer diagnoses and generally has a poor prognosis due to its aggressive nature. About 15% of patients have brain metastases at initial diagnosis, with the prevalence rising to over 50% within 2 years. Early identification is critical in guiding treatment and improving patient outcomes. Brain metastases can be difficult to identify in young patients with non-specific neurologic symptoms. Although cystic brain lesions raise concern for infectious etiologies, metastatic disease should always be considered.
Conclusions: This case highlights the importance of caution when caring for patients with often stigmatized conditions, such as psychiatric diseases and substance use disorders. Clinicians should beware of diagnostic momentum when patients have characteristic findings on radiologic studies and maintain a broad differential diagnosis.