Background: In the late 1990s, the hospitalist role emerged in the United States, and the effectiveness of hospitalists in improving healthcare quality and patient safety has been demonstrated. Due to a shortage of medical personnel for inpatients, Korean government initiated hospitalist programs starting in 2016. The patient care model focused on inpatients by surgical specialists is referred to as the surgical hospitalist program(SHP), this study aimed to investigate the effectiveness of SHP in improving postoperative outcomes and healthcare costs for inpatients, in comparison with traditional surgical patient care models.
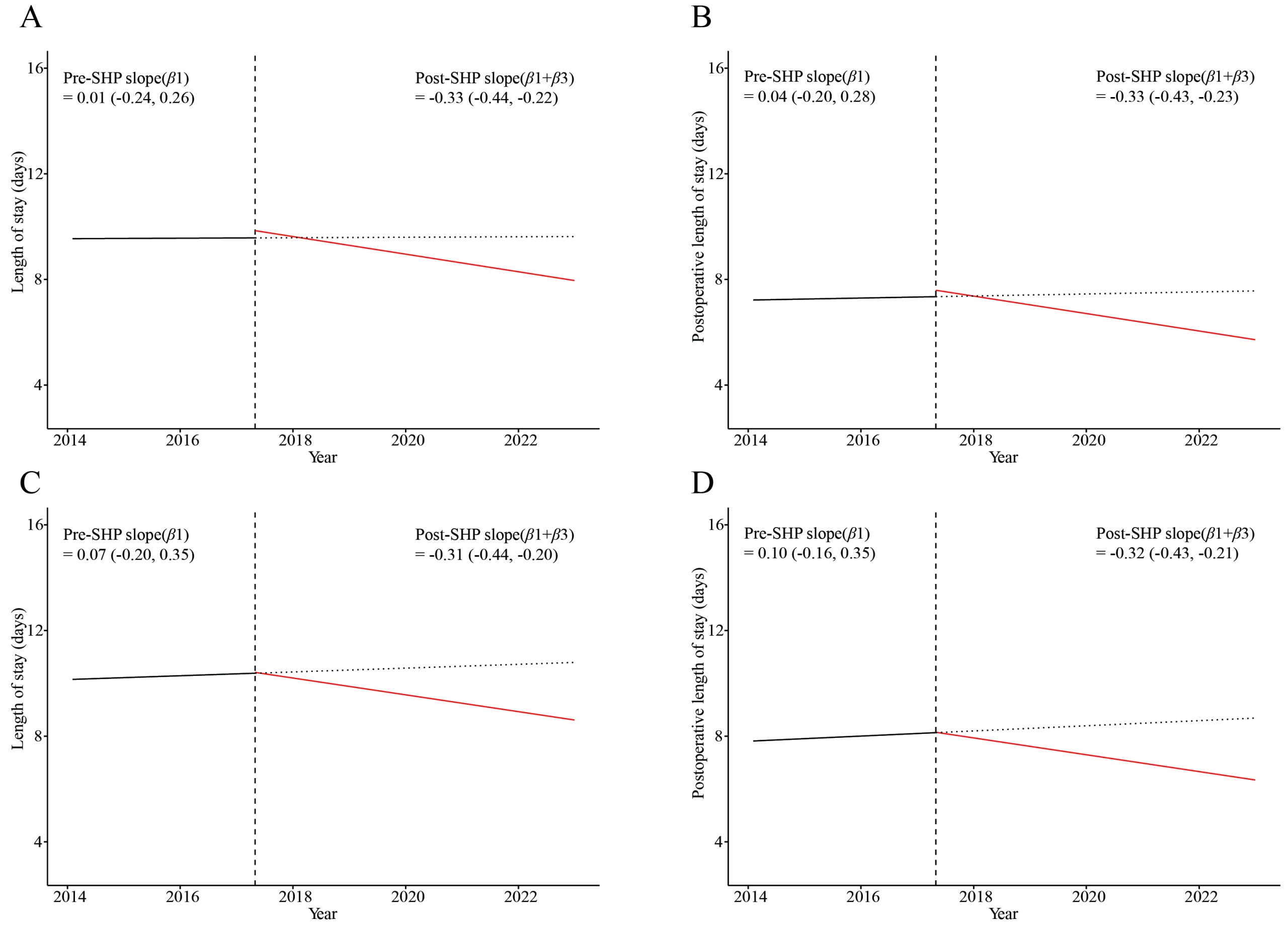
Methods: A retrospective cohort study was conducted on patients who underwent surgery from 2014 to 2022 in the Division of Colorectal Surgery and Gastrointestinal Surgery. The study compared postoperative outcomes and healthcare costs before and after the implementation of the SHP across each division. Specifically, it utilized interrupted time series analysis to compare changes in trends of each outcome before and after SHP implementation. Additionally, the study examined the impact of varying degrees of surgical hospitalist involvement on postoperative outcomes.
Results: The study found that surgical hospitalists absorbed between 25% to 58% of each division’s patient census, and there was a noticeable shift of patients with critical illness from residents to surgical hospitalists after the implementation of the SHP. Despite an increase in patient severity and a corresponding rise in postoperative complications after the SHP’s implementation, regression analysis showed that SHP introduction was associated with a reduction in postoperative length of stay across all divisions. Specifically, SHP implementation correlated with reduced ICU transfers, re-operations, and readmissions within 30 days in the Division of Colorectal Surgery, decreased occurrences of complications grade 3a and above in the Division of Gastrointestinal Surgery. The ITSA results indicated that after the introduction of the SHP, there was a significant decreasing trend in postoperative complications and hospital-acquired infections across all divisions. Additionally, the SHP appeared to counteract the increasing trend in hospital costs. And it was found that when surgical hospitalists cared patient for more than 50% of the total hospital stay, there was a significant impact on reducing the length of stay and improving postoperative outcomes.
Conclusions: The aging of surgical patients, increasing severity of conditions, and a decrease in healthcare personnel focusing on inpatients are significant contributors to the worsening outcomes of surgical patients. The findings support the adoption of hospitalist models in surgical care to enhance efficiency, improve patient care quality, and optimize resource use. The expansion of the surgical hospitalist program with more surgical hospitalists is likely to become a key factor in enhancing the quality of healthcare for surgical patients.