Background: Mounting evidence supports the use of point-of-care ultrasound (POCUS) in medicine and pediatrics to improve outcomes, maximize patient safety, and increase patient satisfaction and success of procedures.The literature describes the utility of POCUS in several areas of pediatric care (the emergency department, pediatric and neonatal intensive care unit, and post-acute care setting), however, we are unaware of prior case series or studies of POCUS to guide management specifically among hospitalized children.General pediatricians have not widely adopted procedural or diagnostic POCUS and few pediatric residency programs offer robust POCUS exposure to trainees, with only 17% of recently surveyed programs reporting having a formal POCUS curriculum.We seek to illustrate the range and impact of POCUS within our children’s hospital by describing a series of cases that included use of POCUS to guide or change management.
Methods: This was a retrospective case series of patients who underwent POCUS for clinical purposes while admitted to our 150-bed quaternary care children’s hospital between February 2018 to July 2024. This study was exempted from review by the Institutional Review Board of UNC (IRB 23-2277). This case series included 74 children who presented to the pediatric emergency department or inpatient service during the study period and had a POCUS examination completed by a physician who may have been participating directly in their care or consulted to perform a specific POCUS exam or procedure. Patients were identified for inclusion in this study if their POCUS examination changed or guided management or a procedure. Eight patients were excluded from the case series after their POCUS examination was not found to change their plan of care.
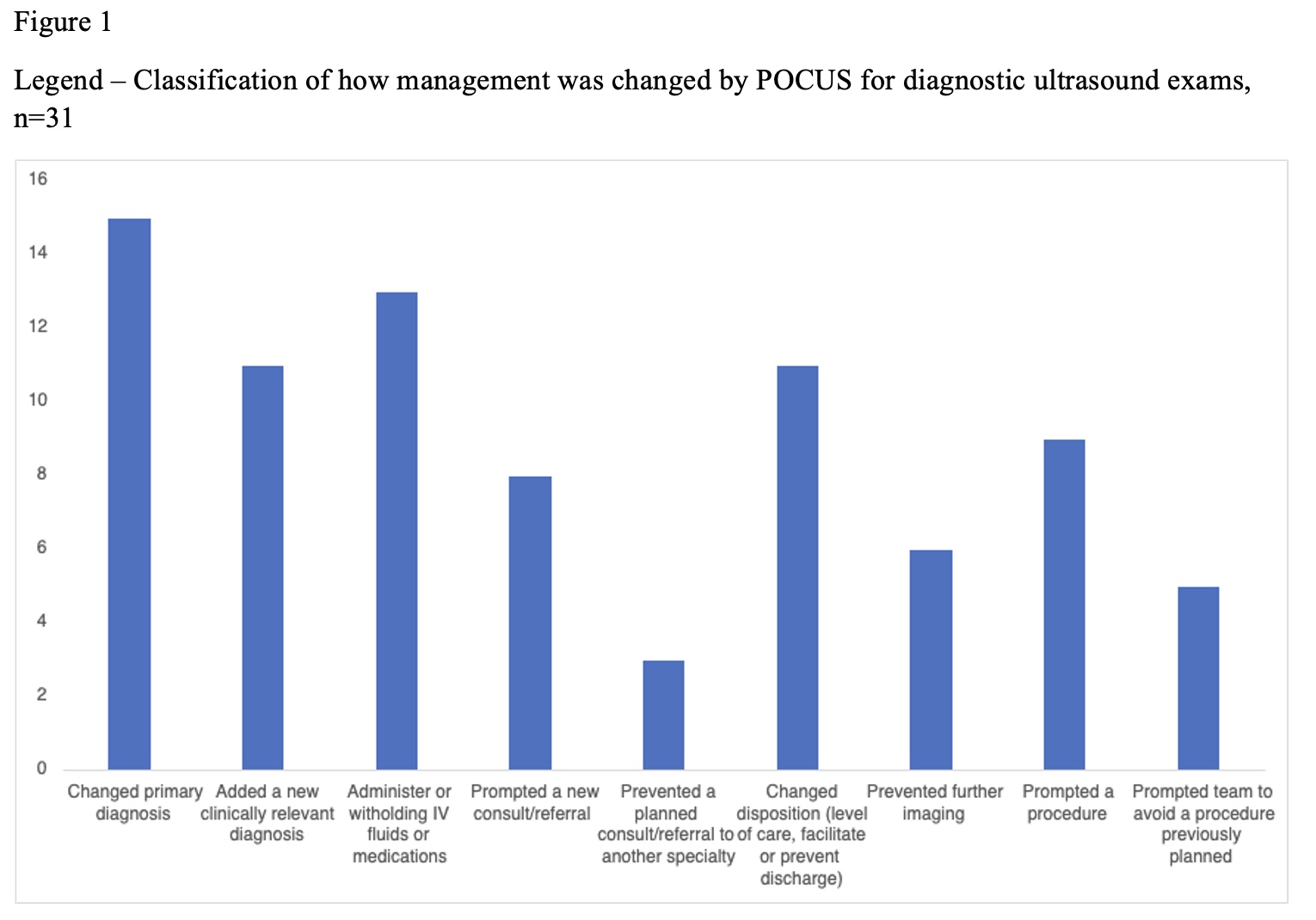
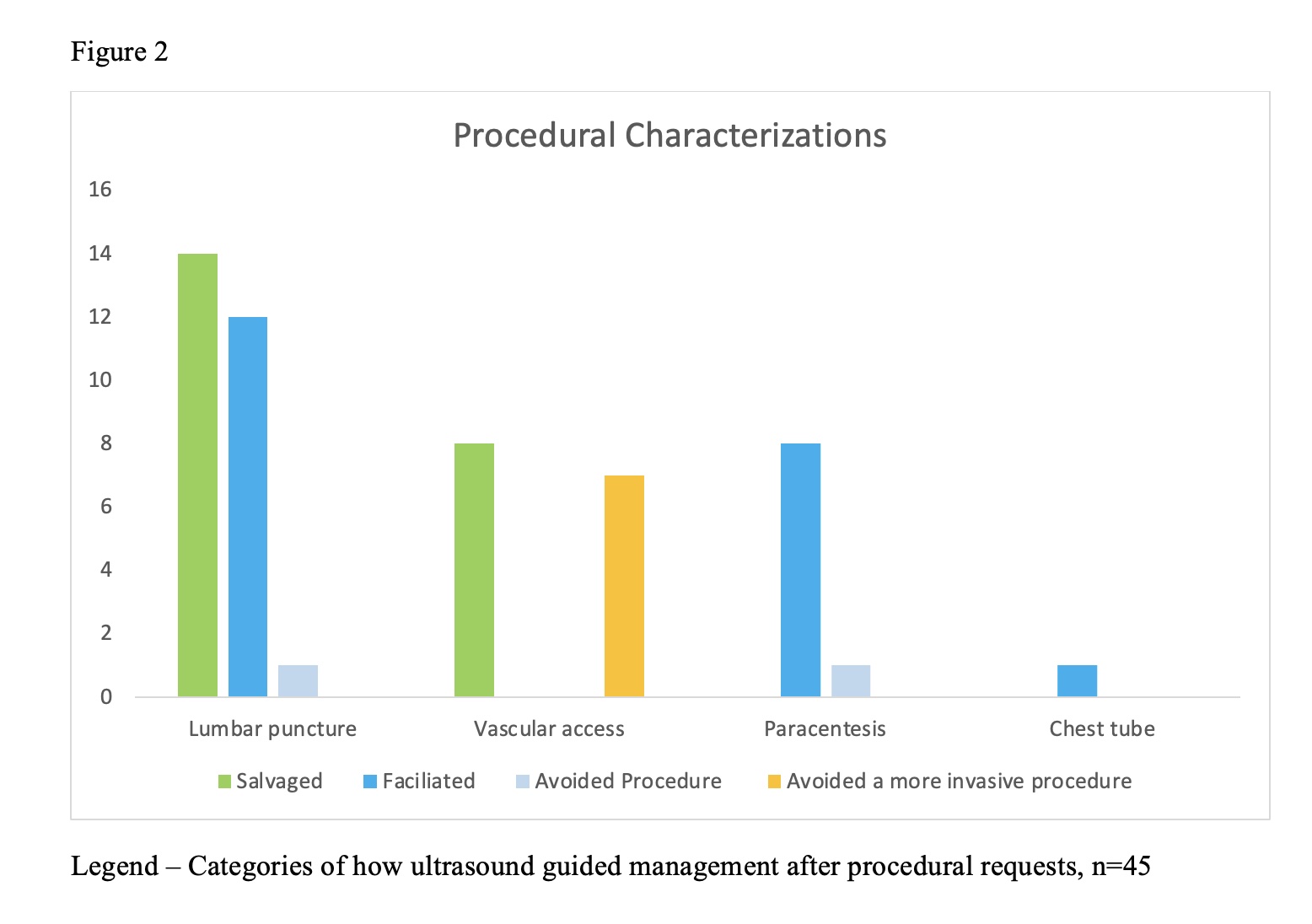
Results: We identified 66 patients (Mean age was 8.3 years) who had 76 POCUS examinations during which ultrasound changed management or guided a procedure.For diagnostic POCUS, 31 POCUS exams were performed on 29 patients. The most frequent organ systems examined were pulmonary (38%), genitourinary/renal (21%), abdominal (13%), and cardiac (13%). Figure 1 shows the classification of how POCUS changed management across all organ systems examined. The most frequent change in management was a change in primary diagnosis in 13/31 exams (41.9%). A total of 45 procedures were performed on 37 patients (including 8 repeat procedures). Lumbar puncture (60%), paracentesis (20%), and vascular access (18%) were most commonly performed. As shown in Figure 2, ultrasound led to successful procedures in children who had undergone prior unsuccessful attempts without ultrasound and spared children the placement of unnecessary central venous catheters. Additionally, two children were spared from procedures (a lumbar puncture and paracentesis) that would not have yielded fluid.
Conclusions: We describe ultrasound applications in a hospitalized general pediatric population and their immediate impact at the point of care. Our results should serve as an impetus for more widespread adoption of POCUS in general pediatrics and for integration of POCUS training into pediatric residency programs by demonstrating its practical value to patient care.