Background: Discharge planning plays a critical role in managing hospital length of stay (1). We report on the implementation of a program in a large hospital system where health care providers were requested to estimate and record the Medically Ready for Discharge Date (MRDD) in the electronic health record (EHR) for hospitalized patients to facilitate discharge planning. MRDD was defined as the date when acute hospital needs had resolved, and the patient was considered clinically stable to move to a lower level of care. New metrics for discharge delays, unnecessary bed hours (UBH) and days (UBD), were tracked as the difference between actual discharge date and last MRDD value. The primary aim was to evaluate the association between MRDD entry timing and UBD. Secondary aim was to evaluate other factors associated with UBD.
Methods: Discharges for 112,930 patient visits from 4 hospitals between 01-January-2021/31-July-2022 were evaluated. Detailed subgroup analysis was conducted for 33,771 Medicine and Pediatric patients. Descriptive statistics were used to report MRDD utilization and patient population characteristics. Multivariable regression models and tree-based machine learning methods were used to control for medical, demographic and operational characteristics to estimate factors associated with UBH and UBD.
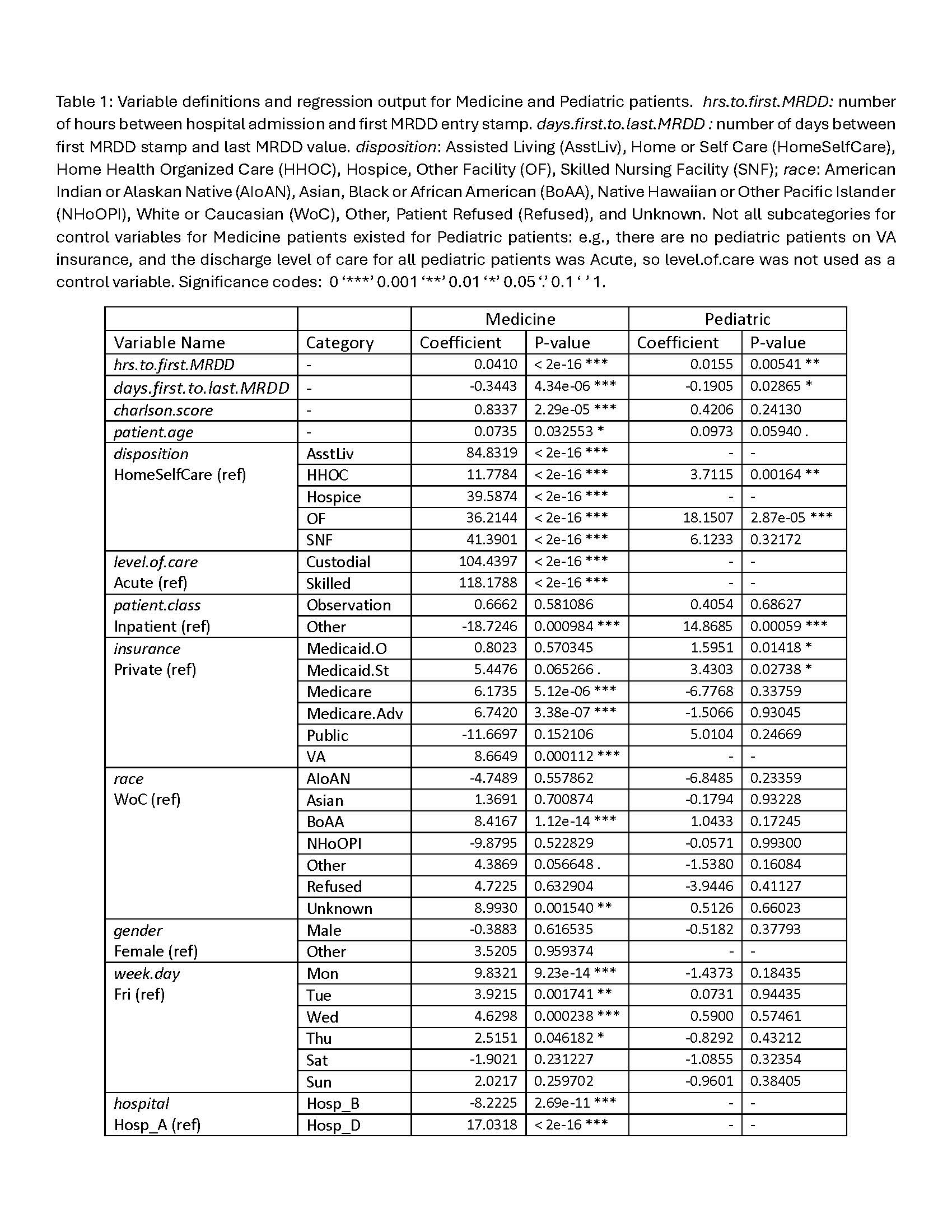
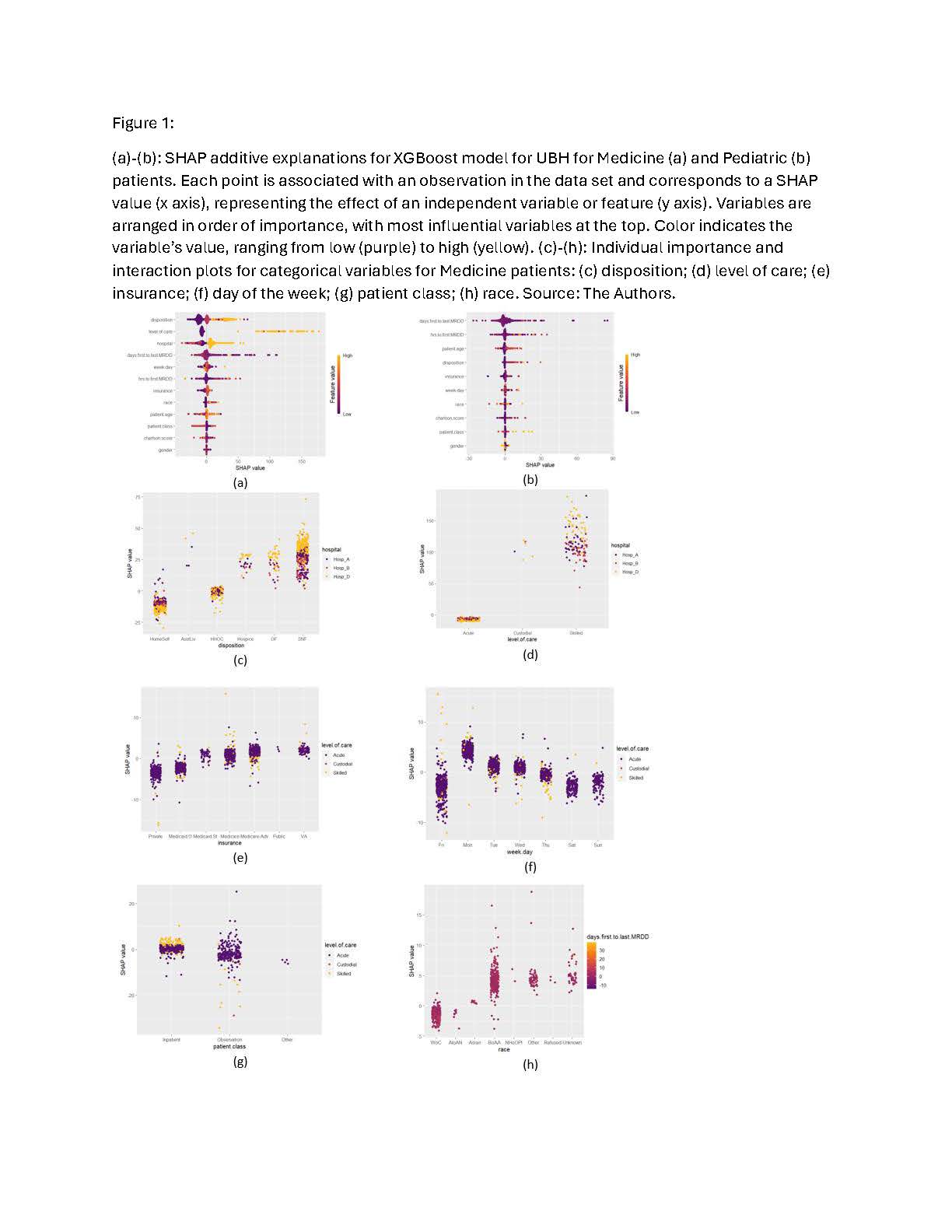
Results: The subgroup regression output analysis for Medicine and Pediatric showed that the longer the time to the first MRDD entry, the longer the UBH. Each additional hour after hospital admission it takes to enter the MRDD contributes 0.04 UBH for a Medicine patient, i.e., an additional day increases UBD by one hour (Table 1). These observations are confirmed by the XGBoost model (Fig. 1). The longer the time between the first MRDD entry time stamp and the last MRDD value, the shorter the UBD. Delaying MRDD entry for Medicine patients by one day is associated with 1351 UBD, or 3 years of unnecessary bed days. Disposition, level of care, insurance, and day of week are significant for predicting UBD. The average UBD for patients going to Assisted Living, Skilled Nursing Facilities, Hospice, and Other Facilities (84.83, 41.39, 39.59, and 36.21 additional hours, respectively) were significantly higher than in Medicine patients discharged home. Medicine patients with VA, Medicare Advantage, Medicare, and Medicaid State insurance require 8.66, 6.74, 6.17 and 5.45 more UBH than Medicine patients with private insurance. The largest number of discharges and the shortest UBH occur on Friday. Relative to Friday discharges, Monday discharges are associated with 9.83 more UBH.
Conclusions: A statistically significant decrease in UBD was associated with earlier predicted MRDD entry. This “advanced notice” for when a patient will be medically ready allows for more coordinated care amongst the interdisciplinary team. The impact of saved unnecessary bed days in a capacity constrained health care system equates to millions of dollars saved. The novel application of tree-based machine learning algorithms confirmed by multivariate regression analysis makes this work an important contribution to the field. Our findings support health care systems implementing coordinated discharge planning with MRDD forecasting early during the hospitalization for efficient patient throughput with decreased unnecessary bed days.