Background: Inequitable healthcare is delivered to those who are incarcerated and have a history of incarceration. Incarceration has a significant multiplicative impact on the health of those who experience it – worsening outcomes related to chronic illness and shortening life expectancy. Hospital based providers tend to interact sporadically with individuals who are incarcerated, limiting the opportunity to develop expertise and knowledge in care differences for this population. Kaiksow et al describe 7 domains of healthcare for people who are hospitalized in the setting of incarceration including decreased provider engagement, privacy violations, impaired patient autonomy, fewer medical interventions, continuous shackled restraints, limited environmental control, and impaired transitions of care.
Purpose: We sought to address the co-existing challenges of lack of medical school curricular attention to patients who are incarcerated or have a history of incarceration, as well as deficiencies in knowledge, skills, and attitudes in caring for these patients among hospital-based medical providers.
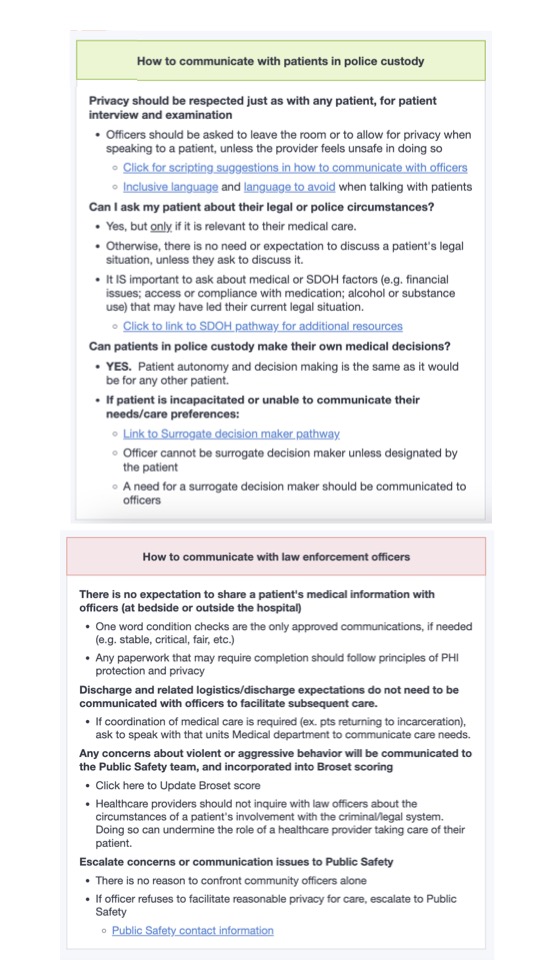
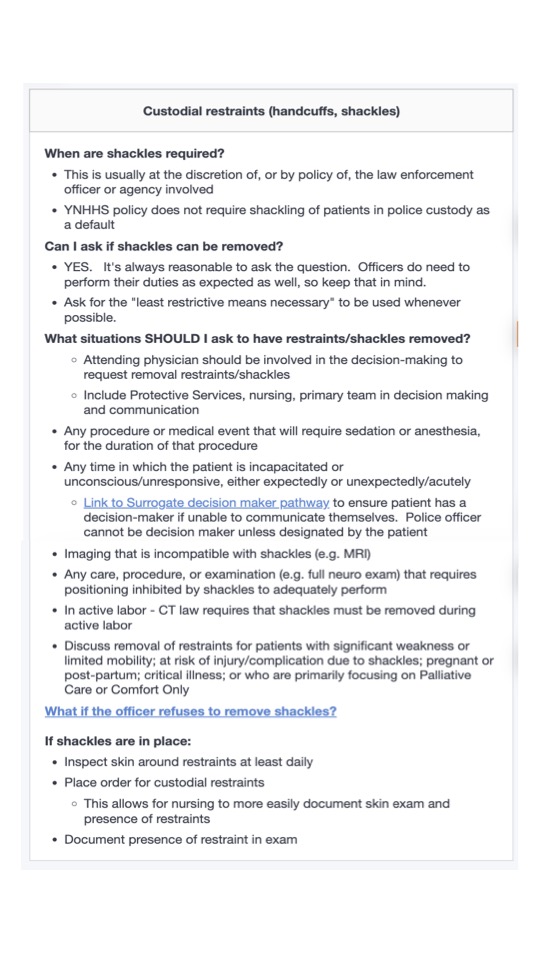
Description: Beginning in September 2023, the Association of American Medical Colleges (AAMC) funded Yale School of Medicine to partner with a local community-based organization, Women Against Mass Incarceration (WAMI), as part of an education grant entitled, “The DePART Initiative: Detained Patients’ Advocacy and Rights throughout Treatment.” The first phase resulted in a medical education event entitled “Accountability to the Community” that was featured as part of Yale’s Interprofessional Longitudinal Clinical Experience (ILCE) course, where students pursuing education to become nurse practitioners, nurse midwives, physicians, and physician associates learn alongside each other. The day culminated with a listening session and qualitative needs assessment with both community experts and faculty. The data generated from this session, as well as iterative focus groups, resulted in the development of a patient bill of rights and Yale’s Care Signature Pathway for Incarcerated Patient Care.The pathway took the form of four sections which map to the domains described in Kaiksow et al: General Guidance, Communication, Patient Care, and Discharge. The General Guidance section begins with a Patient’s Rights section with links to the YNHHS Patient Rights and Cooperation with Law Enforcement policies. The Communication tab includes descriptions of how to communicate effectively and privately with patients, with recommended language to use with law enforcement personnel to ensure this (Figure 1). The Patient Care section focuses primarily on custodial restraints – delineating that it is always reasonable to request shackle removal, including specifying the “least restrictive means necessary” (Figure 2). The Discharge tab focuses on identifying medications on formulary at the carceral facility, scheduling follow up appointments prior to discharge, and ensuring social work engagement.
Conclusions: Our Pathway for Incarcerated Patient Care will ensure that clinicians have the information they need to provide optimal equitable care, and advocate for the health needs, communication needs, and fundamental rights of their hospitalized patients. Our current version maps to the expressed needs of our collaborative partners – those with lived experience of hospitalization while incarcerated, as well as to the themes described in available published expert opinion and clinical experience on this topic.