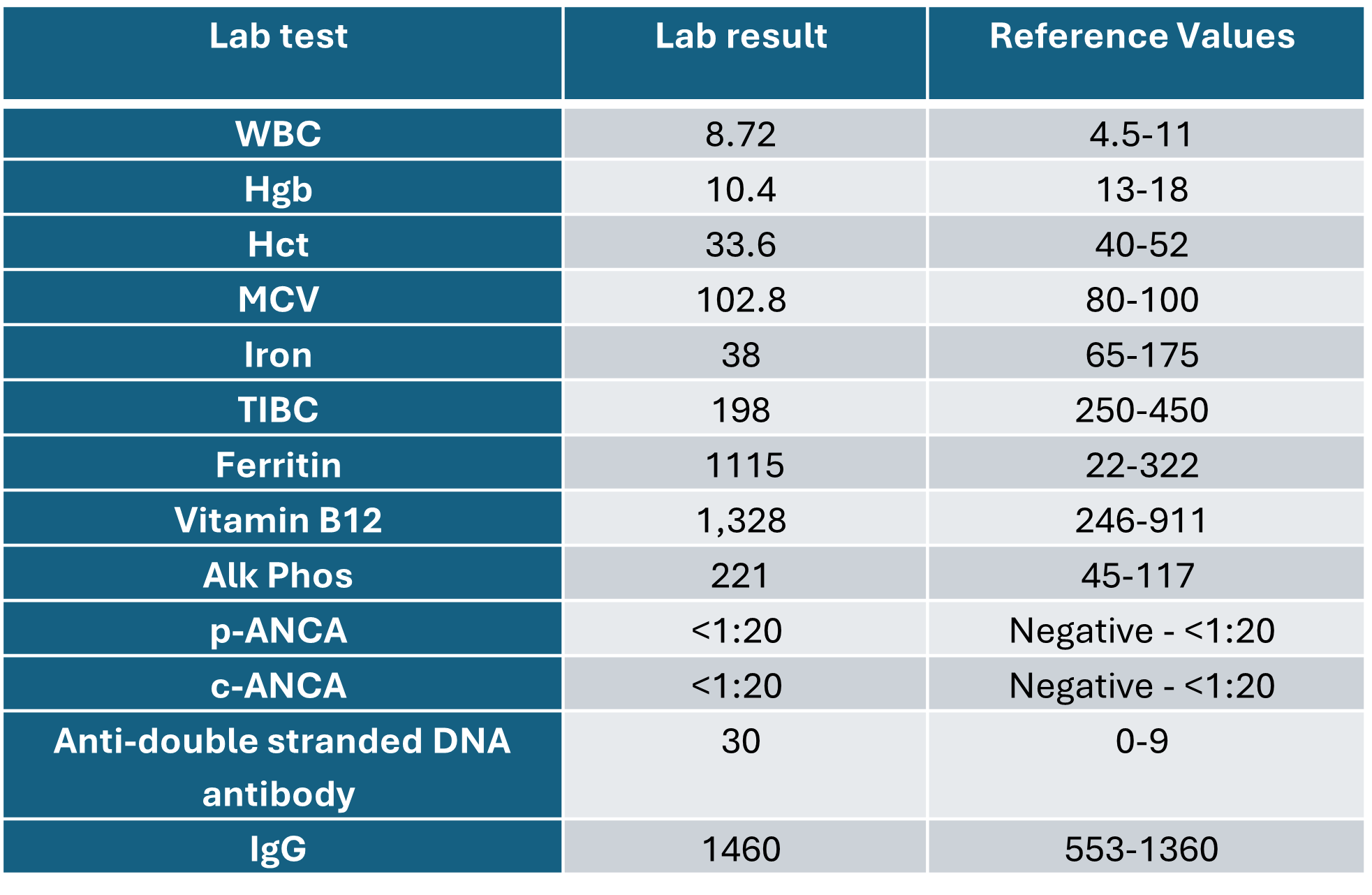
Case Presentation: A 64-year-old man presented with persistent anemia, weight loss, fatigue, fever, cough, episcleritis, chondritis, and facial pain. Initial investigations highlighted macrocytic anemia and elevated alkaline phosphate. Despite initial suspicion of a streptococcal infection and subsequent treatment with antibiotics, his condition did not improve. Further evaluation revealed cavitary nodules on chest imaging, with biopsies confirming granulomas with cryptococcal organisms. He was treated with a 12-month course of Voriconazole. However, his symptoms persisted along with a recurrent rash every 2 weeks. Detailed serologic evaluation for systemic autoimmune diseases was unremarkable besides a positive anti-double stranded DNA antibody and positive rheumatoid factor. Bone marrow biopsy revealed myeloid hyperplasia with vacuoles. Patient was transferred for immunology evaluation resulting in a diagnosis of VEXAS syndrome with UBA1 gene mutation detected by Sanger Sequencing. Treatment with prednisone and Bactrim led to notable improvement, and he remains on the JAK inhibitor, Ruxolitinib.
Discussion: A recent breakthrough revealed a single somatic mutation linking myelodysplastic syndromes and autoimmunity. VEXAS syndrome, a myeloid-driven autoinflammatory condition associated with hematological neoplasms, was first described in 2020. It stems from somatic mutations in the UBA1 gene, causing diverse hematological and rheumatic symptoms. These include skin lesions, fever, chondritis, arthritis, and thrombosis. Currently, the treatment options of VEXAS include immunosuppressive drugs such as corticosteroids and methotrexate, cytokine targeting agents, JAK2 inhibitors, and the hypomethylating agent azacytidine. However, the efficacy of these agents remains unclear, and treatment is considered challenging due to multi-organ involvement, variability in presentation, often accompanied by hematological malignancies, reliance on glucocorticoids, and resistance to traditional immunosuppressive treatments.
Conclusions: Patients with autoimmune symptoms and no clear diagnoses may challenge clinicians. Early consideration of VEXAS syndrome could be crucial. Our case report highlights the potential benefits of prompt diagnosis and targeted anti-inflammatory treatment. Despite its recent characterization, VEXAS is seen as a progressive condition with frequent relapses and potential harm from both the disease and its treatments.