Case Presentation: A 58-year-old man with a history of type 2 diabetes mellitus (A1c 9.1%), recurrent ear infections presented to hospital with left ear pain, facial weakness, and sudden vision loss. The patient had frontal and left-temporal headaches for several months thought to be secondary to migraines or temporal arteritis. A temporal biopsy had been scheduled, and he received 5 days of high-dose prednisone. Six weeks prior, he developed left-sided facial weakness diagnosed as Bell’s palsy and treated with 7 days of acyclovir and prednisone. Ten days previously, he received ciprofloxacin drops for left otitis externa. At current presentation, he had persistent symptoms and sudden left visual loss. Examination was notable for left facial droop, an afferent left pupil deficit, and complete restriction of left extraocular movements. His inflammatory markers were elevated (ESR>140, CRP 104). Brain MRI showed skull base osteomyelitis extending into the internal auditory canal, a left mastoid effusion, and enhancement of the left orbital apex and left optic nerve. The patient was admitted and started on broad spectrum antibiotics. A head MRA was normal, and a head MRV showed partial thrombosis of the left sigmoid sinus and jugular bulb/superior aspect of the left internal jugular vein. Heparin was initiated. ENT was consulted, but there was no area safe to biopsy. Lumbar puncture showed 20 WBCs/uL (73% lymphocytes), and elevated CSF protein (88mg/dL). Liposomal amphotericin B and voriconazole were started due to concern for an invasive fungal infection. Later, the CSF beta-D Glucan assay returned elevated (101 pg/mL). He had a negative cryptococcal CSF antigen, negative urine histoplasma antigen, negative serum aspergillus antigen, and a negative CSF fungal culture. The patient was ultimately diagnosed with malignant fungal otitis externa complicated by cervical and skull base osteomyelitis, otomastoiditis, and sigmoid and internal jugular vein thrombosis, suspected to be due to aspergillus. Upon review, the patient had grown a fungal organism during an episode of otitis externa one year prior. He had a known ruptured left tympanic membrane (TM) and worked in a sawmill. Due to the extent of disease and location, antifungals alone were not curative, and surgical debridement was not possible. The patient was discharged to home hospice.
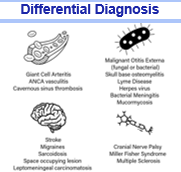
Discussion: This case highlights the diagnostic challenges of malignant otitis externa (MOE). The patient had risk factors including uncontrolled diabetes, work exposures, and a perforated TM. His symptoms were misdiagnosed as Bell’s palsy, migraines, and temporal arteritis, leading to delayed diagnosis and neurological consequences. While most MOE is caused by Pseudomonas, fungal MOE represented 15% of cases at a tertiary referral center2. Fungal MOE often occurs after prolonged exposure to antibiotics. Fungal MOE has over an 11% mortality rate and severe morbidity including cranial nerve palsies, skull base osteomyelitis, thrombosis, and pseudoaneurysm 1,3.,4.
Conclusions: This case underscores the importance of avoiding early anchoring bias and revisiting assumptions. In this case, there were several opportunities to evaluate further prior to multiple cranial nerve palsies developing. It is important to recognize that Bell’s palsy is a diagnosis of exclusion and every patient with facial nerve palsy and alarm symptoms or poorly controlled diabetes should receive a comprehensive evaluation for malignant etiologies.