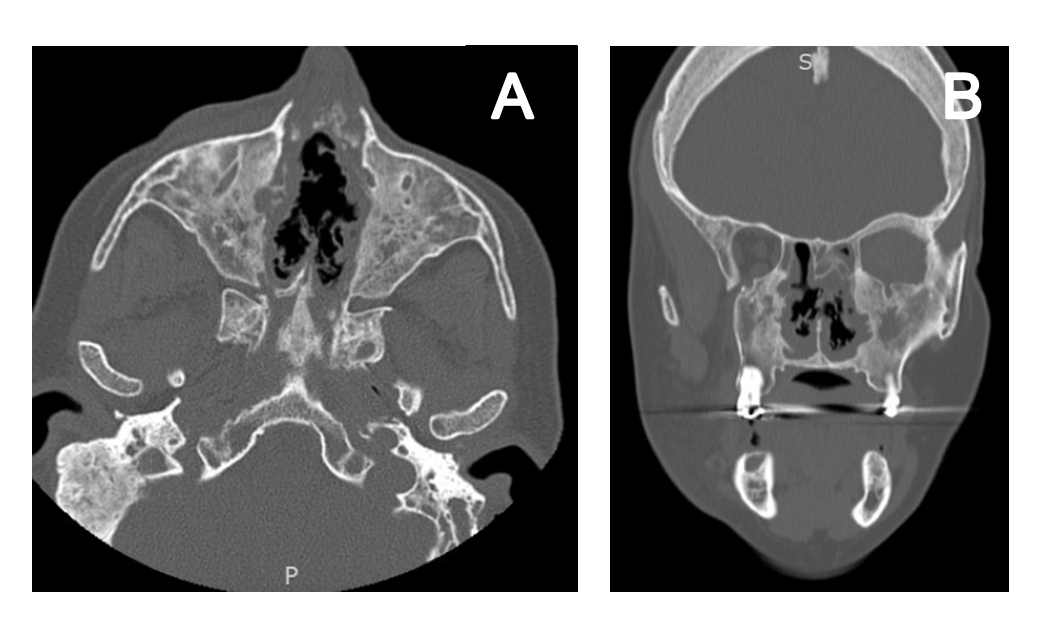
Case Presentation: A 56-year-old female with a history of recurrent MRSA sinusitis and c-ANCA and PR3 positive granulomatosis with polyangiitis (GPA) presented with right-sided facial droop sparing the eye and upper face, unilateral facial numbness, and right-sided tongue deviation that began four hours before presentation. She also endorsed sinus fullness for the past three days but denied fever, headache, speech difficulty, and focal weakness. A code stroke was activated, although she was outside the window for thrombolytics. Non-contrast CT head and MRI brain showed pansinusitis without signs of ischemia or hemorrhage (Figure 1). White blood count was consistently normal throughout the admission, although ESR and CRP were elevated to 50 mm/hr and 3.36 mg/dL, respectively. Respiratory cultures grew MRSA and ESBL E. Coli, prompting initiation of vancomycin and meropenem. Her immunosuppressive regimen of methotrexate, azathioprine, and annual rituximab infusion was held until antibiotics were completed. Over five days, her facial droop, tongue deviation, and numbness resolved. She was discharged after completing seven days of IV antibiotics, and she then resumed her immunosuppressive regimen. Since this admission, she continues to endorse chronic sinusitis but denies other GPA symptoms (e.g., hematuria, hoarseness, coughing, joint pain) and has not since had any pseudo-stroke episodes.
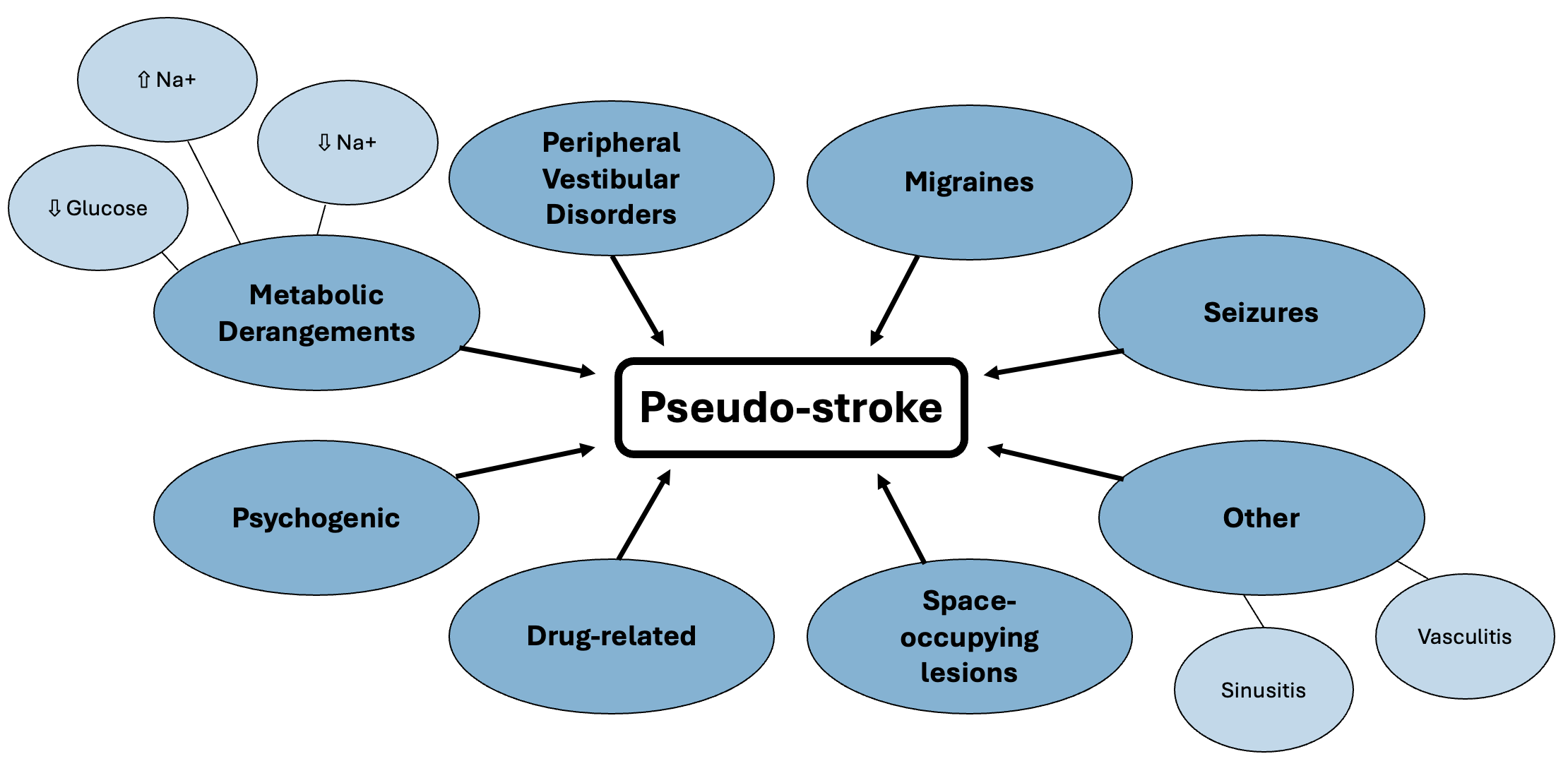
Discussion: Pseudo-stroke refers to acute onset focal neurological dysfunction that is found to have a non-vascular origin. Common causes of pseudo-stroke include peripheral vestibular disorders, seizures, metabolic derangements and migraines. Given our patient’s prior GPA diagnosis, other less frequent causes were considered, including mononeuritis multiplex, cerebral vasculitis, and bacterial sinusitis. (1–3) Initial stroke workup should be performed in all stroke-like presentations; however, if this is unrevealing, it is important to then begin workup for alternative causes of pseudo-stroke. (4)In this case, mononeuritis multiplex secondary to GPA flare and bacterial sinusitis with direct extension were the leading differential diagnoses. Peripheral sensory and motor impairment, including mononeuritis multiplex, can occur in up to 50% of patient with GPA with up to 40% of case involving cranial nerves. (2,3) When this happens, patients typically have active GPA symptoms, which our patient lacked. (5) The treatment of choice includes immunosuppressive agents such as cyclophosphamide, steroids, and rituximab. (2,3,5–7) Our patient’s presentation resembled mononeuritis multiplex involving cranial nerves V and VII but symptoms resolved without any immunosuppression.Acute and chronic sinusitis can compress intracranial structures potentially resulting in cranial nerve palsies and a pseudo-stroke presentation. (8,9) To resolve both the infection and inflammation, a patient-specific antibiotic regimen is the treatment for sinusitis. (8) Although both mononeuritis multiplex and bacterial sinusitis were considered possible causes of pseudo-stroke in this patient with a history of GPA, her symptoms resolved with antibiotics alone, suggesting sinusitis as the etiology.
Conclusions: The resolution of this patient’s symptoms with antibiotics highlights bacterial sinusitis as a cause of pseudo-stroke. This case emphasizes considering stroke mimics and using treatment response and follow-up as key diagnostic tools.