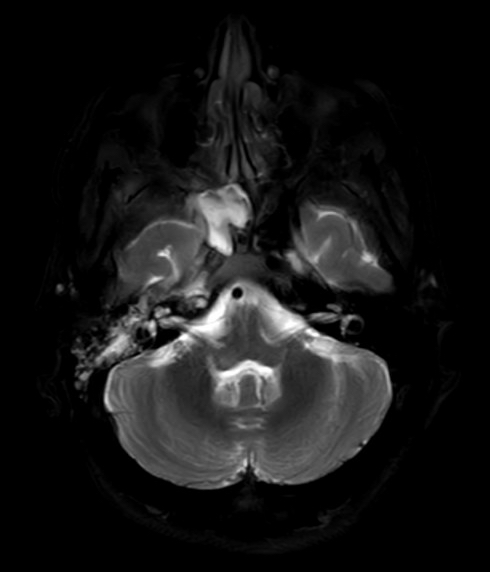
Case Presentation: An 18-year-old female with type 1 diabetes presented with odynophagia and neck pain. She was previously admitted for a culture-negative peritonsillar abscess treated with surgical incision and drainage (I&D), amoxicillin-clavulanate, and hydrocortisone. Admission diagnosis was diabetic ketoacidosis (DKA). CT neck demonstrated extension of fluid into the right retropharynx and surrounding the right internal carotid artery, resulting in complete occlusion of this vessel and development of inflammatory intraluminal thrombus. She was intubated, started on linezolid, cefepime, and metronidazole, and admitted to the ICU. The patient underwent repeat surgical I&D, which grew Candida albicans and few respiratory florae. Antibiotics were narrowed to ampicillin-sulbactam and fluconazole. Although the patient’s inflammatory markers initially improved, she continued to experience severe neck pain. She underwent a third I&D, from which cultures grew Saccharomyces cerevisiae. Histopathologic examination of retropharyngeal tissue demonstrated necrosis and granulation tissue extending to the surrounding skeletal muscle and blood vessels, concerning for aspergillosis vs. mucormycosis. Microbial cell-free DNA testing identified Rhizopus arrhizus and confirmed the diagnosis of mucormycosis. The patient was started on liposomal amphotericin B. Subsequent CT neck demonstrated angioinvasive disease and skull base osteomyelitis. In multidisciplinary care discussions, the mortality risk of aggressive debridement/resection of infected tissue outweighed the very low likelihood of cure. The patient elected to continue life-prolonging therapy with IV amphotericin and was discharged home with hospice care. The patient eventually died from complications of her infection four months after diagnosis.
Discussion: Mucormycosis is a rare, life-threatening fungal infection, most commonly affecting diabetic and immunosuppressed hosts. It typically presents with rhino-orbito-cerebral infection through inhalation of fungal spores and often initially appears clinically similar to bacterial sinusitis. Mortality of rhino-orbito-cerebral infection is estimated between 25-73% and up to 96% in patients with disseminated disease. Diagnosis of mucormycosis is challenging due to frequently unsuccessful culture growth, often resulting in delayed treatment. In 2021, the prevalence of diabetes mellitus was 11.6% of the U.S. population. In children and adolescents aged younger than 20 years, the incidence of both type I and type 2 diabetes increased significantly between 2008 and 2018. Given the rising incidence of diabetes among the growing population of the U.S., it is important for physicians to consider mucormycosis early for diabetic patients admitted with symptoms of underlying infection. Early consideration and diagnostic testing for Mucor and Rhizopus species can significantly reduce mortality for these patients.
Conclusions: The purpose of this case is to describe a rare and fatal case of mucormycosis originating from a retropharyngeal abscess in an 18-year-old patient with type I diabetes. This case was complicated by angioinvasive disease, resulting in compressive occlusion of the right carotid artery with eventual infection of the skull base. It is important for hospital physicians to consider mucormycosis early in diabetic and immunocompromised patients admitted with infectious symptoms, beyond those specific to rhino-orbito-cerebral disease.