Case Presentation: The patient was a 61-year-old female with a medical history of hypertension, type II diabetes mellitus, and uterine carcinosarcoma with peritoneal carcinomatosis, and ascites who initially presented with abdominal pain and shortness of breath. Admission labs were significant for a white cell count of 15.6 and lactic acid of 2.6. Sepsis workup was initiated and she was started on broad-spectrum antibiotics. Abdominal and Pelvic imaging did not reveal any definitive source of infection. Despite adequate fluid resuscitation and broad-spectrum antibiotics, her lactic acid levels remained elevated. Due to her hemodynamic stability and negative blood cultures, antibiotics were discontinued. Liver function tests were normal, suggesting that lactic acidosis was likely secondary to malignancy and the Warburg effect. However, her Riboflavin level was found to be < 5 (normal range: 6.2-39 nmol/L). She was started on daily Riboflavin supplementation, which ultimately resolved her lactic acidosis, and she was discharged home.
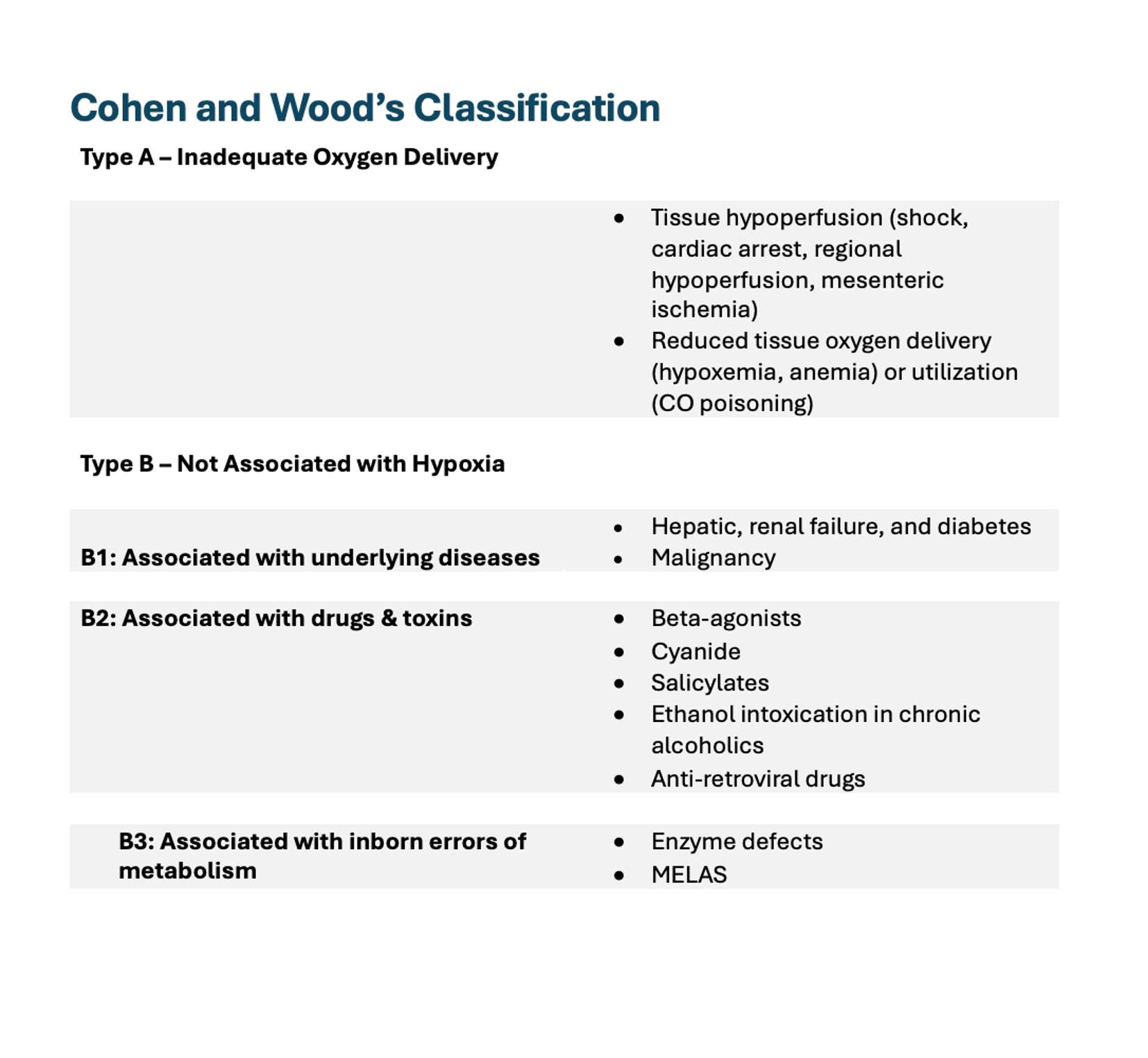
Discussion: Lactic acidosis is broadly divided into 2 major types: type A caused by tissue ischemia leading to anaerobic metabolism and excessive lactic acid production, and type B caused by impaired cellular metabolism and lactic acid buildup without tissue hypoperfusion. There are some less common types such as type D caused by intestinal overproduction and type B3 caused by congenital enzymatic deficiencies.Type A lactic acidosis is the most common and dangerous type due to its association with life-threatening conditions such as hypoxemia and shock. Type B lactic acidosis is less common but can indicate serious underlying issues such as hematologic and solid organ malignancies, as well as liver failure. Other causes of type B lactic acidosis include thiamine or riboflavin deficiency, alcoholism, toxic alcohol, and medications such as metformin, linezolid, propofol, and IV epinephrine. Vitamin deficiencies, though often overlooked, can cause lactic acidosis in hospitalized patients, potentially leading to misdiagnosis of sepsis and unnecessary antibiotic use. Our patient had lactic acidosis secondary to Riboflavin deficiency. Riboflavin, a water-soluble vitamin, is essential for the coenzymes flavin mononucleotide and flavin adenine dinucleotide. A deficiency disrupts cellular metabolism and mitochondrial energy production, resulting in impaired pyruvate metabolism and lactic acid accumulation. Severe deficiency can cause systemic mitochondrial dysfunction, manifesting as myopathies and seizures. It is important to note that HAART therapy with nucleoside analogues can lead to Riboflavin deficiency, which in turn can cause lactic acidosis. Treatment with oral or intramuscular supplementation typically resolves symptoms quickly.
Conclusions: Vitamin deficiencies, though often overlooked, can cause lactic acidosis in hospitalized patients, potentially leading to misdiagnosis of sepsis and unnecessary antibiotic use. Thiamine and Riboflavin are the two most common vitamin deficiencies associated with type B lactic acidosis. Daily intake of fruits and vegetables rich in Riboflavin is enough to meet the body’s requirements. Deficiency commonly occurs in patients with poor appetite and malnutrition. HAART therapy with nucleoside analogues can lead to Riboflavin deficiency, which in turn can cause lactic acidosis.