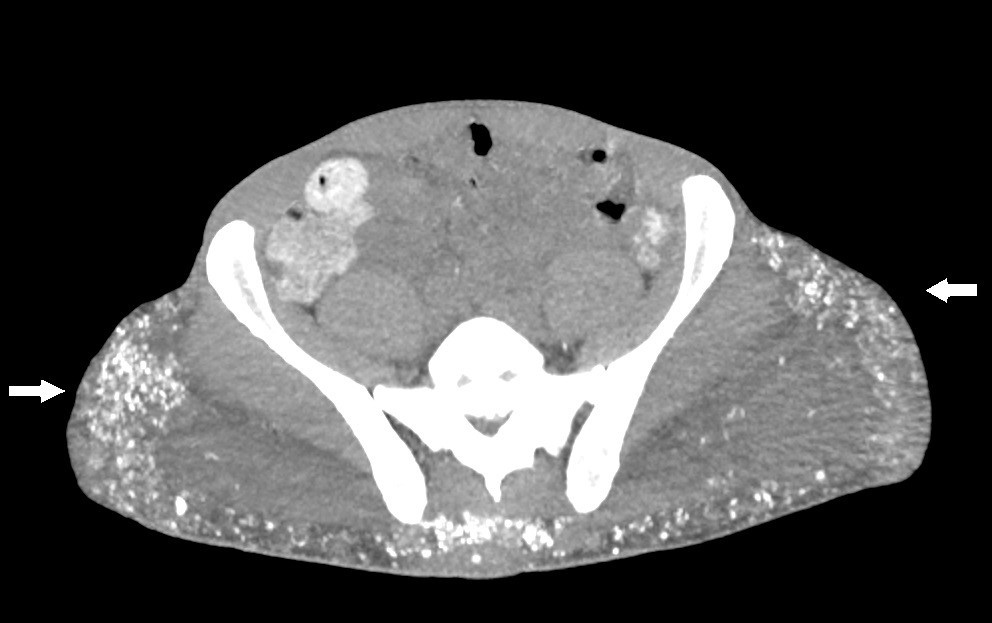
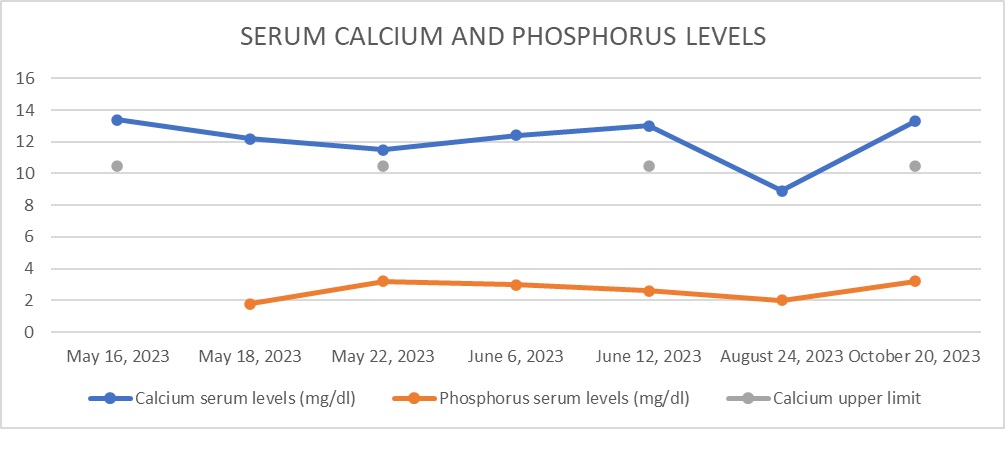
Case Presentation: A 44-year-old African American male with a medical history of human immunodeficiency virus (HIV) and chronic kidney disease (CKD) presented to the hospital with nonspecific complaints, including flank pain. Initial laboratory tests and imaging studies confirmed a diagnosis of nephrolithiasis and acute kidney injury with concomitant hypercalcemia. The patient was hospitalized and treated with intravenous fluids and pamidronate, which led to the normalization of calcium levels. Further investigation of the hypercalcemia revealed an inappropriately normal parathyroid hormone (PTH) level for the degree of calcium elevation. Additional diagnostic workup, including a computed tomography (CT) scan, revealed hyperlucent deposits in both gluteal regions. Upon questioning, the patient revealed a history of silicone injections administered 20 years earlier, raising the suspicion of exogenous overproduction of 1,25-dihydroxyvitamin D. Following treatment, his calcium levels improved, and he was advised to continue outpatient follow-up. However, one month later, he was readmitted with recurrent hypercalcemia. Due to the complexity of managing hypercalcemia in the context of CKD, the nephrology team recommended initiating denosumab, as bisphosphonates are not an appropriate medication in patients with impaired renal function. After receiving the first dose, the patient’s calcium levels improved; however, he was lost to follow-up before the second dose could be administered.
Discussion: Silicone is known to be a rare cause of hypercalcemia, often years after its administration as part of cosmetic procedures. In 1964, Winer et al. described three biopsy-proven cases of granuloma formation after silicone injection, naming them “siliconomas” [1]. They observed siliconomas with a polarized microscope, noting the presence of crystals in the tissue. This constitutes the initial evidence of silicone’s role in causing this phenomenon. The exact mechanism of this granulomatous response is not completely understood but is thought to be similar to what happens in sarcoidosis-induced granulomas [2, 3]. A recent systematic review in 2018 by Tachamo et al. described 23 cases of patients (mostly female) who had received silicone, polymethylmethacrylate, or paraffin oil, and years later developed hypercalcemia [4]. Diagnostic tools like CT scans or PET fluorodeoxyglucose (FDG) are useful in the evaluation of granulomatous diseases like sarcoidosis or amyloidosis and in the diagnostic and prognostic evaluation of malignancies [5]. Currently, there is no definitive treatment for silicone-induced hypercalcemia. Many available case reports [1, 4, 6-11] used strategies like hydration, bisphosphonates, and systemic steroids as the most common management. In our patient, due to his chronic kidney disease, bisphosphonates were not an appropriate first-line therapy, and for this reason, the managing endocrinologist considered denosumab for his outpatient therapy.
Conclusions: This case emphasizes the need for clinicians to consider calcinosis universalis in the differential diagnosis of hypercalcemia, particularly in patients with a history of cosmetic interventions. Prompt identification and accurate diagnosis are essential for optimal management and preventing potential complications.