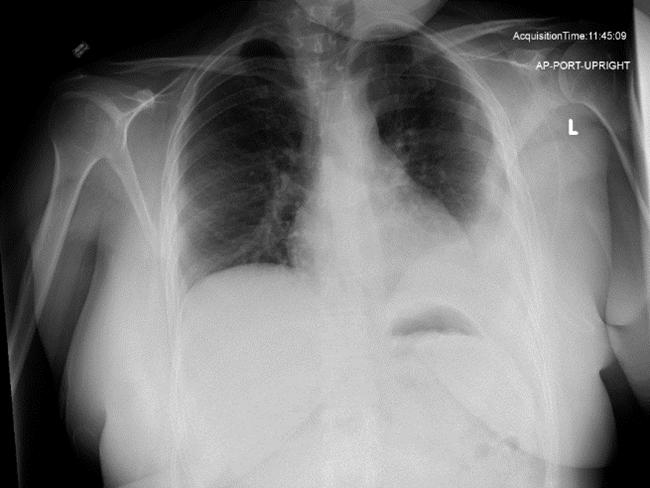
Case Presentation: A 36-year-old female with history of recurrent pleural effusion presented with worsening shortness of breath. One year prior, she was treated for presumed aspiration pneumonia after a moderate left pleural effusion and left lower lobe consolidation were noted on imaging. Initial ultrasound-guided thoracentesis revealed transudative pleural fluid, resolving her symptoms. Despite repeated therapeutic thoracenteses over the course of one year, for recurrent effusions, her condition persisted. A chest X-ray eventually revealed shunt tubing, and further history uncovered a ventriculopleural shunt (VPLS) placed over 25 years ago for hydrocephalus due to ependymoma surgery in early childhood. The shunt’s presence had been missed due to absent records and unclear history. Given the small but stable left lower pleural effusion and slit-like ventricles noted on the MRI, it was determined that the VPLS was functioning, and no acute intervention was required. However, with recurrent effusions, she was managed conservatively with acetazolamide before undergoing definitive surgery to revise the VPLS to a ventriculoperitoneal shunt (VPS). Follow-up imaging showed no pleural effusion, and the patient remained asymptomatic.
Discussion: Extracranial shunts alleviate symptoms in patients with hydrocephalus by diverting cerebrospinal fluid (CSF) to an extravascular compartment.The most common procedure is ventriculoperitoneal shunting (VPS), which is widely used regardless of the underlying cause of hydrocephalus.However, certain patients with multiple shunt revisions, morbid obesity, or a history of abdominal surgeries, may not be suitable candidates for VPS. In these cases, VPLS may be considered as an alternative route for CSF diversion when the peritoneal cavity is unsuitable. Pleural effusions, shunt obstruction, pneumothorax, and empyema have complicated the course of these shunts, but have been infrequent. The mechanisms for accumulation of pleural effusions with VPLS remain speculative. Two hypotheses may explain the development of hydrothorax as a complication of VPLS: (a) impaired pleural absorptive capacity due to pleural damage secondary to prior infection and/or chronic exposure to CSF. (b) excessive drainage of CSF into the pleural space. Most reports of pleural effusions have been in young adults and children, especially within 3 years of placement. A small, asymptomatic pleural effusion visible on chest X-ray indicates that the VPLS is functioning but does not necessarily imply dysfunction. Pleural fluid analysis usually reveals a clear, transudate-like fluid. Asymptomatic or minimally symptomatic effusions warrant close follow-up, while therapeutic thoracentesis can be used as a temporary measure for large symptomatic effusions. Carrion et al. demonstrated that the administration of acetazolamide reduces CSF production, potentially increasing tolerance to VPLS and reducing respiratory symptoms.
Conclusions: Although VPLS insertion is uncommon, it is occasionally utilized in patients with contraindication to VPS. Clinicians should be aware of the possibility of pleural effusions complicating the course of these shunts, which may present even several years later. Shunt revision may be necessary in such cases for definitive treatment.