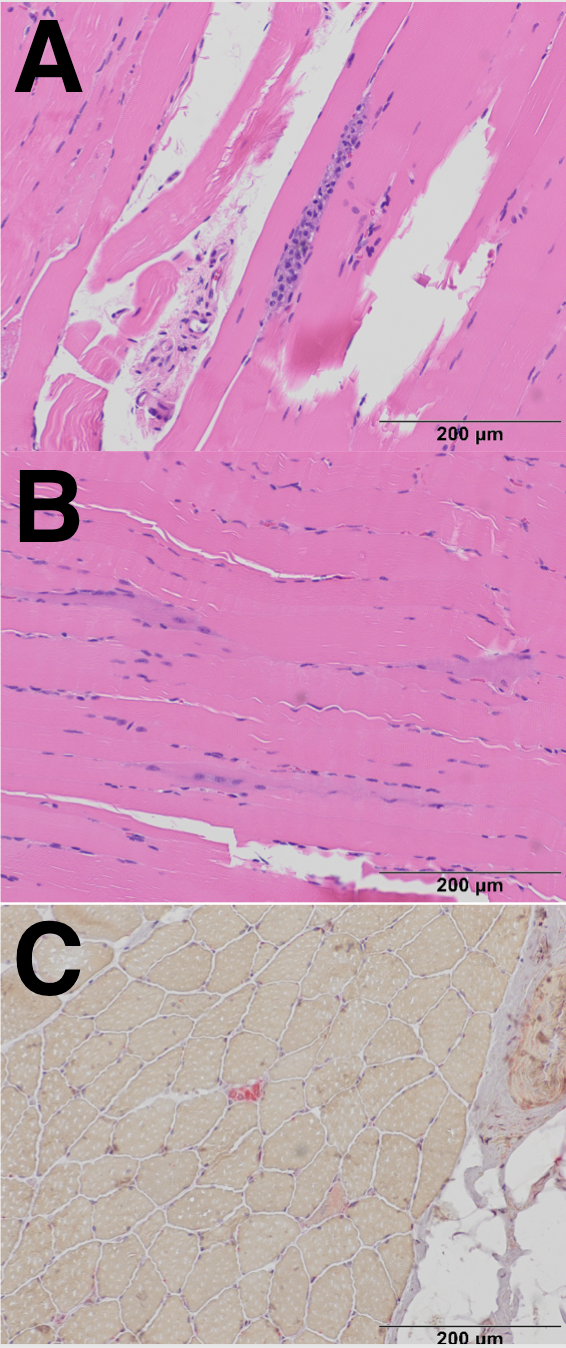
Case Presentation: A 55-year-old woman with a history of hyperlipidemia and hypothyroidism presented with a one month of proximal muscle weakness in her arms and legs, and ten-pound unintentional weight loss. Eight months earlier, routine labs showed mild elevations in ALT and AST levels to ~90. Her atorvastatin was discontinued; however, her liver enzymes continued to worsen over the following months. A liver ultrasound was unremarkable. One month prior to her ED visit, ALT and AST levels had risen to over 300. She presented to the ED with worsening weakness but without synovitis, arthralgias, fevers, ulcers, or photosensitivity. On physical examination, her strength was noted to be 3/5 in both her upper and lower extremities. Lab results showed a CPK greater than 15,000 U/L, positive ANA, positive SSA, and an elevated HMG CoA receptor IgG of 143 units (reference range 0-19). MRI of her extremities demonstrated muscular edema consistent with nonspecific myositis. Muscle biopsy (Figures A, B, C) revealed myonecrosis with myophagocytosis and minimal lymphocytic inflammation.The patient was diagnosed with immune-mediated necrotizing myopathy (IMNM) and received two doses of IVIG. She was discharged on a prednisone taper and twice-monthly IVIG infusions, with follow-up arranged with rheumatology.
Discussion: Immune-mediated necrotizing myopathy (IMNM) is a type of necrotizing myopathy characterized by minimal inflammatory infiltrates on biopsy. There are three subtypes of IMNM: anti-SR, anti-HMGCR autoantibody, and seronegative. Our patient has the anti-HMGCR subtype, which can occur in both statin-exposed and statin-naïve individuals. Its incidence among statin users is 2-3 per 100,000. The duration of statin use before symptom onset varies, ranging from six months to three years, and some patients develop myopathy even after discontinuing the statin. Atorvastatin is most commonly implicated. Clinically, IMNM presents with subacute proximal limb muscle weakness and elevated CK levels. Some patients may experience pharyngeal muscle involvement, leading to symptoms such as hoarseness and dyspnea. It is essential to rule out other antibodies, such as anti-Ro52, anti-PM-Scl, and antimitochondrial (AMA), among others.Statins are contraindicated in patients with statin-associated IMNM. Treatment typically begins with glucocorticoids and IVIG, which is often continued for years. In non-severe cases, alternative immunosuppressive therapies, such as steroids with methotrexate, azathioprine, or mycophenolate, may be considered. Monitoring CK, CBC, and CMP levels is important, and MRI can be useful in assessing muscular edema. Patients should also undergo physical rehabilitation. Notably, statin-naïve, anti-HMGCR-positive IMNM patients more frequently require third-line therapy (50% versus 9%) and have worse outcomes, including higher rates of severe or fatal outcomes (50% versus 0%).
Conclusions: Hospitalists should recognize statin-associated immune-mediated necrotizing myopathy as a potential cause of rhabdomyolysis with a subacute onset. This condition is unresponsive to intravenous fluid administration and presents with proximal muscle weakness in patients on statin therapy who have no prior history of autoimmune disease.