Case Presentation:
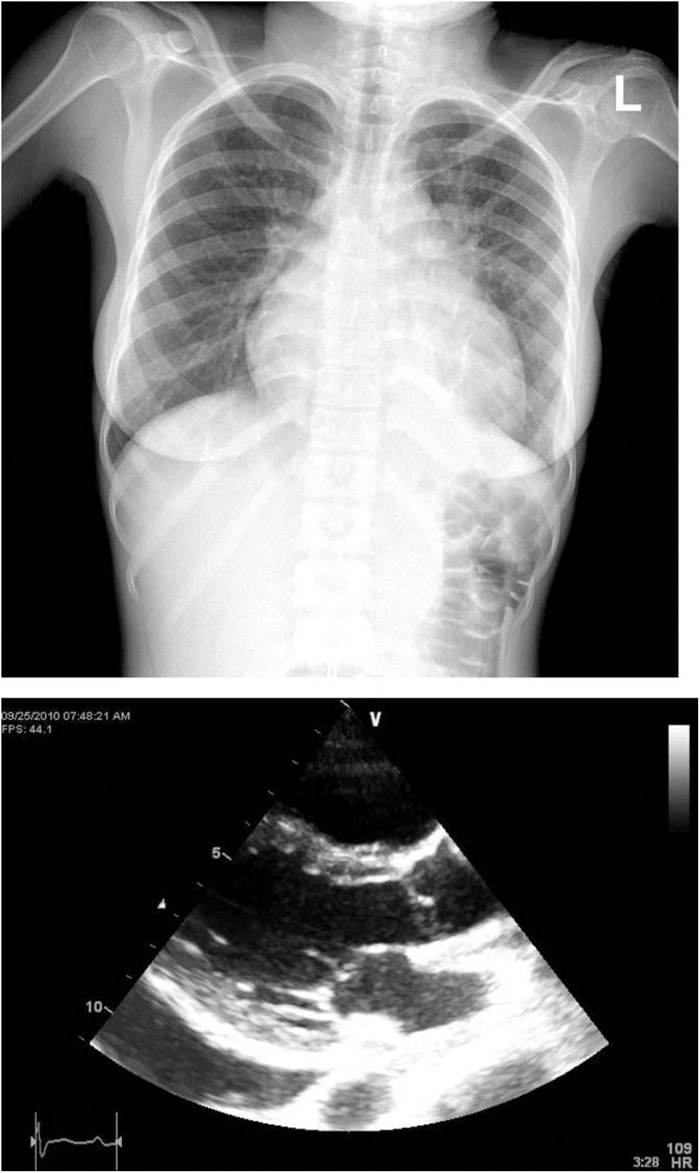
A 20‐year‐old woman presented with 2 weeks of worsening dyspnea, pleuritic chest pain, and dry cough. She was previously healthy. No weight loss, night sweats, fevers, or chills were reported in the past. New abdominal right upper quadrant pain started 2 days prior to admission. Initial vital signs revealed tachycardia of 125, increased jugular venous pressure, and tender liver. Pulsus paradoxus was negative. A scratchy, high‐pitched sound was heard over her left chest. Sedimentation rate was 86, with reactive thrombocytosis, hypoalbuminemia, and normocytic anemia. HIV serology and autoimmune workup were negative. Electrocardiogram revealed sinus tachycardia with nonspecific ST‐T‐wave changes. Enlarged globular heart and left‐sided small pleural effusion were noted on the chest x‐ray. Hilar and mediastinal lymphadenopathy were described on chest CT. Echocardiogram revealed a moderate to large pericardial effusion without tamponade physiology. Pericardiocentesis drained only 300 cc of bloody fluid, suggestive of loculation. There were no malignant cells reported on cytology. The patient was a native of Ethiopia who had immigrated to the United States 7 months prior to admission. Empirical 4‐drug therapy was started for a concern of tuberculous pericarditis. A paratracheal lymph node biopsy revealed necrotizing poorly defined granulomas. After 3 weeks, sputum and paratracheal lymph node biopsy cultures grew Mycobacterium tuberculosis.
Discussion:
Tuberculous pericarditis is occasionally seen in United States, but it is the most common cause of infectious pericarditis in Africa. Clinical presentation varies. Cough, dyspnea, and chest pain are common symptoms. Only half of patients have night sweats, weight loss, or fever. The onset may be abrupt, resembling acute idiopathic pericarditis, or insidious, resembling congestive heart failure. Ninety percent of patients have an enlarged heart on chest radiograph. As many as 40% also have a pleural effusion. Echocardiography may reveal multiple loculations of pericardial fluid. Bloody fluid suggests either tuberculosis or malignancy. In areas of high endemicity, a presumptive diagnosis is often correctly made, and antituberculous treatment is started empirically. Nucleic acid amplification technique (polymerase chain reaction) for tuberculosis on pericardial tissue has excellent sensitivity and specificity (90% and 100%, respectively) and is a fast method to support the diagnosis; however, culture is still the diagnostic gold standard. Therefore, a diligent search for acid‐fast bacilli in the sputum, lymph nodes, pericardial fluid, and tissue is mandatory.
Conclusions:
Tuberculous pericarditis is serious condition and, if untreated, carries high morbidity and mortality. Despite that it is rarely seen in the United States, it has to be a part of differential diagnosis, particularly in patients coming from an endemic area.
Disclosures:
N. L. Margeta ‐ none