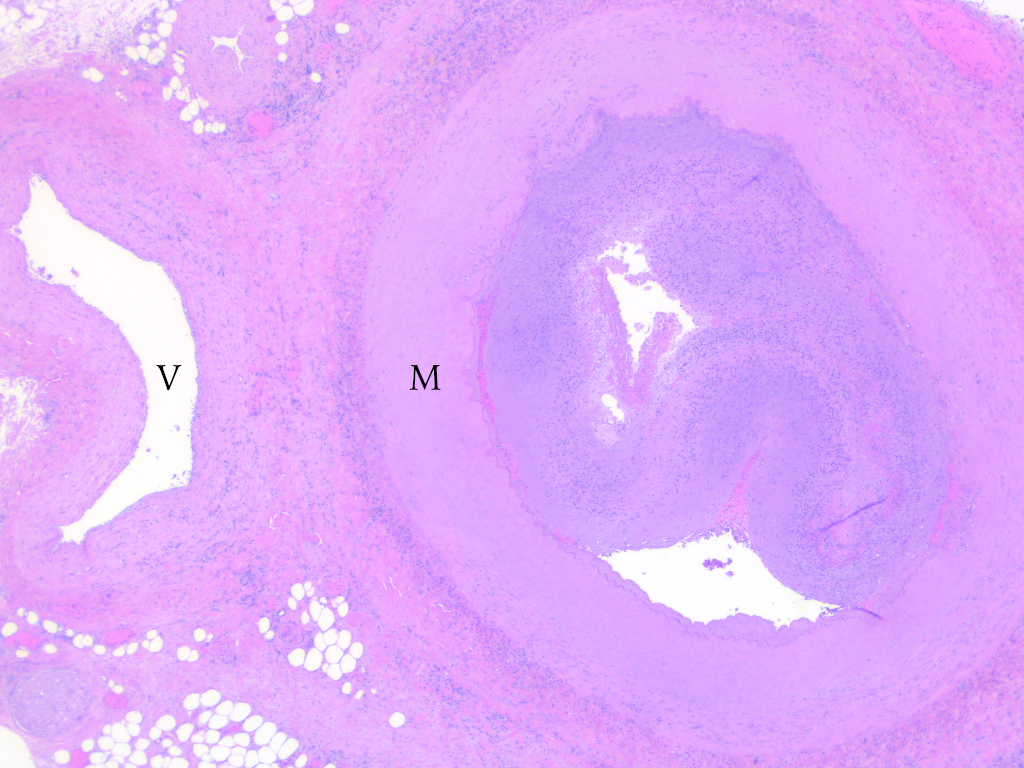
Case Presentation: A 24-year-old previously healthy man initially presented with 2 weeks of fevers, headaches and neck pain. He also reported recent, transient swelling and redness of the right ear, a resolved erythematous rash of all extremities and ongoing, intermittent testicular pain. Work-up revealed elevated ESR and CRP, but normal brain MRI, CSF analysis and CT abdomen/pelvis. He was diagnosed with ice pick headache and fever of unknown origin and discharged with specialist follow-up. Days later, he returned with ongoing fevers, night sweats and lower extremity cramping with ambulation. On admission, he was febrile (38.8°C) and normotensive with a normal exam. Laboratory studies revealed normal kidney function, mild anemia, leukocytosis, thrombocytosis, mild transaminitis and elevated ESR and CRP. Infectious work-up was negative, including HIV and syphilis screens, a hepatitis panel and blood cultures. Autoantibody evaluation was negative aside from a low-positive RF.While hospitalized, he experienced chest pain with an elevated troponin and EKG abnormalities suspicious for myopericarditis. On day 5 of admission, he developed sudden, severe right foot pain with pallor, poikilothermia and absent dorsalis pedis and posterior tibial pulses. Emergent CT angiography (fig. 1) revealed occluded right posterior tibial and bilateral anterior tibial, peroneal and dorsalis pedis arteries as well as irregularities of superior and inferior mesenteric artery branches suggestive of medium vessel vasculitis. High-dose steroids were started, but symptoms progressed to include the left leg. Right thrombectomy, catheter-directed thrombolysis, balloon angioplasty and finally right above-the-knee amputation were performed. Microscopic examination of the leg (fig. 2) showed medium-sized arteries with necrosis of the media and organizing thrombus with sparing of the veins, compatible with polyarteritis nodosa (PAN). Cyclophosphamide was added followed by plasmapheresis, but due to refractory inflammation and ischemia, he also required a left below-the-knee amputation.
Discussion: More common among older patients with peak incidence in the sixth decade of life, PAN is a necrotizing vasculitis of mostly medium-sized arteries with resultant stenoses, thromboses and microaneurysms, which can lead to ischemia, infarction and bleeding. This entity classically presents with systemic symptoms, including fever and weight loss, along with single or multi-organ involvement, especially of the nervous system, skin, gastrointestinal tract and kidneys, commonly sparing the lungs and with marked elevation of inflammatory markers but negative autoimmune serology [1]. PAN presenting with peripheral vascular disease is uncommon, with few case reports describing patients who present with claudication, peripheral gangrene or acute limb ischemia, especially with a disease course as aggressive as our patient, who ultimately required anticoagulation, immunosuppression, plasmapheresis and surgical intervention [2-6].
Conclusions: This case portrays a uniquely aggressive course of a rare disease presenting with uncommon clinical manifestations. For the hospitalist, recognition of claudication even in the young patient without atherosclerotic risk factors is essential with inclusion of primary vasculitides on the differential diagnosis of peripheral vascular disease. Early diagnosis may reduce disease-associated morbidity and mortality by allowing for prompt initiation of immunosuppression.