Background: Despite evidence that the use of medications for patients with opioid use disorder (OUD) leads to reduced mortality and improved engagement in outpatient addiction treatment, these life-saving medications are underutilized in the hospital setting. This study reports the outcomes of a hospitalist-led interprofessional and multidisciplinary inpatient program, known as the B-Team (buprenorphine team), to guide the initiation of buprenorphine and transition to outpatient treatment following discharge.
Methods: The B-Team is notified of patients that may be candidates for buprenorphine through a secure texting platform accessible to any healthcare provider at the hospital. The B-Team prescriber, who is a hospitalist, psychiatrist, or palliative care provider, orders a nurse-driven protocol for buprenorphine initiation. The chaplain offers psychospiritual counseling and the social worker provides counseling and coordination of care. The B-Team partners with a non-hospital-affiliated publicly-funded office-based opioid treatment (OBOT) program that combines primary care with behavioral health programming. A follow-up outpatient appointment is secured prior to hospital discharge. A member of the B-Team with the “x-waiver” certification prescribes buprenorphine as a bridge until the follow-up appointment. Study data were collected using REDCap electronic data capture tools. This program and study received exempt status from The University of Texas Institutional Review Board.
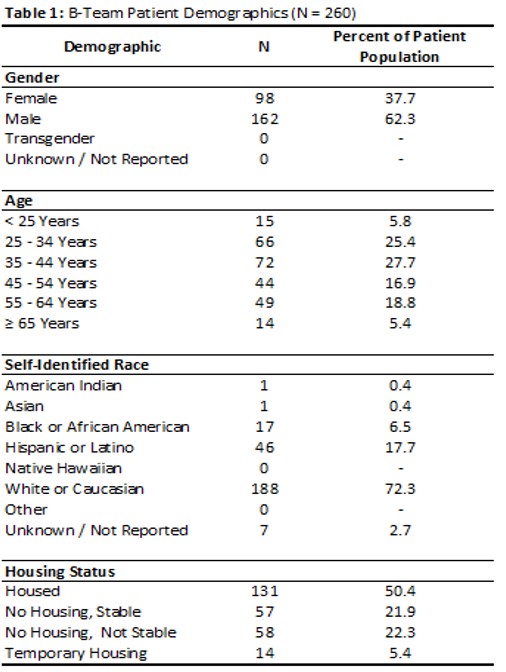
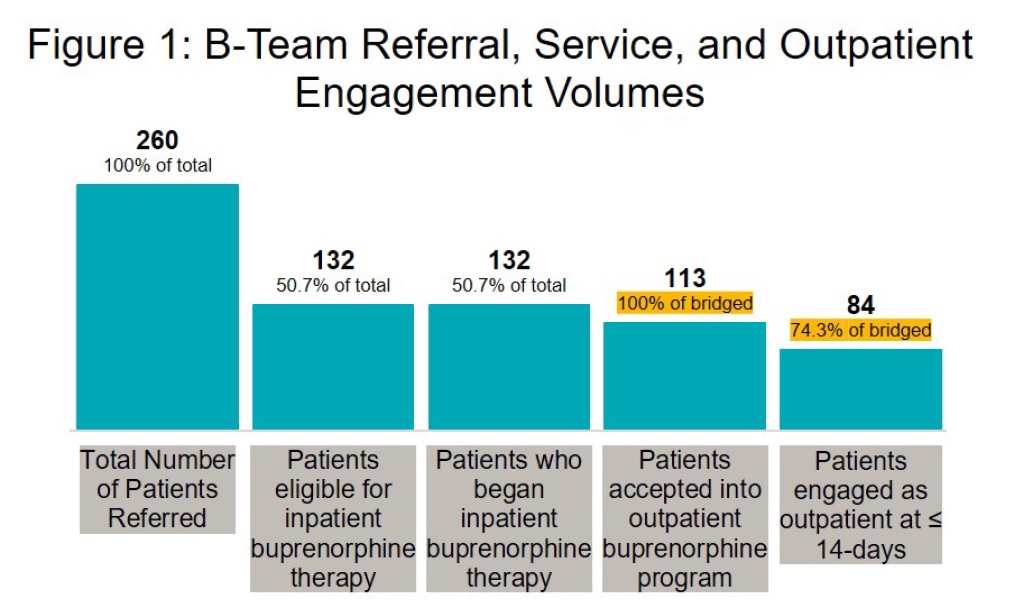
Results: During the first two years, the B-Team received referrals for 260 patients (patient demographics included in Table 1) and began inpatient buprenorphine therapy for 132 patients. Only 5 average monthly inpatient orders for buprenorphine were recorded at this hospital in the year prior to the initiation of the B-Team. Buprenorphine orders increased to 29 per month in the year following the B-Team launch. All 132 eligible patients were seen by a B-Team provider and provided counseling, support, and resources regarding buprenorphine therapy. Of 132 started on buprenorphine therapy during the inpatient stay, 84 patients (74%) were seen at their first outpatient appointment within 14 days (Figure 1).
Conclusions: A hospitalist-led interprofessional team providing evidence-based care for hospitalized patients with OUD led to a substantial increase in patients receiving buprenorphine therapy during hospitalization and at time of discharge. This model is likely to be replicable at other hospitals because it does not rely on dedicated addiction medicine expertise. Moving forward, the B-Team is continuing to establish the treatment of OUD with buprenorphine as the standard of care in the hospital setting. Attending physicians and residents are now encouraged to initiate buprenorphine treatment on their own. In June 2020, we added peer recovery support services to the program, which has been shown to improve care for patients and increase adoption of hospital-initiated SUD interventions. Lessons learned from the inpatient implementation are being applied to the emergency department and an inpatient obstetrics unit at a partner hospital.