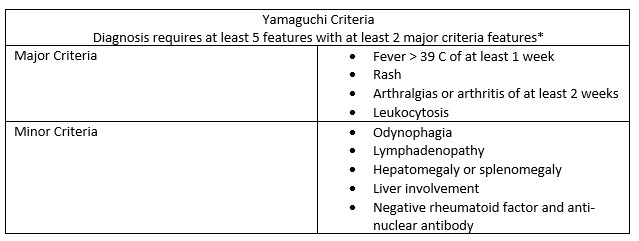
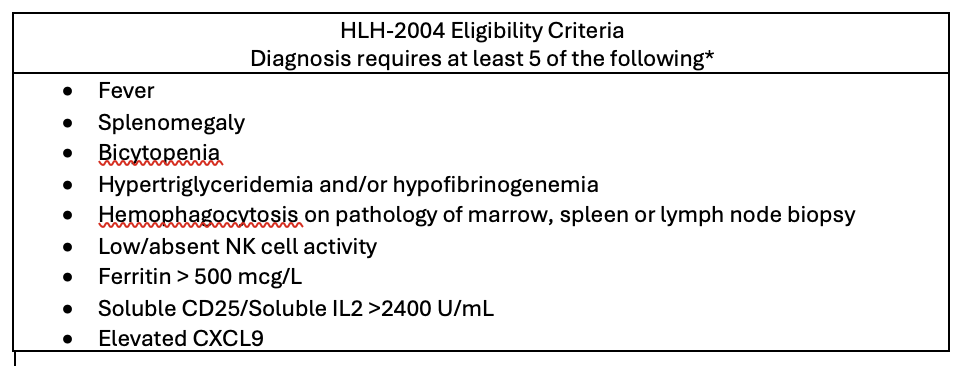
Case Presentation: A 20 year old female with no past medical history presented for fever. She developed fevers, intermittent rash, polyarthralgias and odynophagia prompting her to present to the ED. She was febrile to 38.1 C and heart rate was 126 beats per minute. A faint erythematous facial rash was noted on physical exam along with tenderness in bilateral hands, knees and ankles. WBC was 23.8 K/uL, Hgb 8.5 g/dL and ferritin 11,962 ng/mL. CT neck revealed cervical lymphadenopathy but infectious workup including rapid strep, HIV, EBV, CMV, parvovirus, Lyme and gonorrhea PCR was otherwise negative. Given negative workup and clinical improvement, she was thought to have a post-infectious immune activation syndrome in setting of recent viral illness and antibiotics were discontinued. She was discharged home but fever and rash recurred shortly thereafter causing her to return to the ED. Infectious workup was negative again. IL2, CXCL9 and triglycerides were elevated and ferritin was now 62,472 ng/mL. Given fulfilment of the HLH-2004 criteria (fever, hyperferritinemia, and elevated triglycerides, IL2, and CXCL9), hematology diagnosed her with hemophagocytic lymphohistiocytosis (HLH). Workup for underlying cause of HLH including CT of the chest/abdomen/pelvis, bone biopsy, primary HLH testing, myositis panel and lupus workup was negative. She was started on dexamethasone 20 mg daily with clinical improvement. Given this, she was discharged home with outpatient follow up. She was doing well until her dexamethasone was tapered to 18 mg. She subsequently developed fever and rash again and returned to the hospital, where she was found to have an AST/ALT elevation to 529/376 U/L. Noting she fulfilled Yamaguchi criteria (persistent fever, arthralgias, leukocytosis, pharyngitis, lymphadenopathy with hepatitis) in setting of extensive negative workup of other infectious, oncologic or rheumatologic etiologies, rheumatology diagnosed her with Adult Onset Still’s Disease (AOSD). At this point, both hematology and rheumatology favored a unifying diagnosis of AOSD complicated by MAS (Macrophage activation syndrome). Given inability to taper steroids, she was started on anakinra for treatment of both AOSD and MAS with subsequent significant (and sustained) improvement.
Discussion: AOSD is an inflammatory disorder that classically presents with quotidian fevers, polyarthralgias and evanescent rash. Lymphadenopathy, odynophagia and hepatitis is also common. In retrospect, all of this was present in our patient, yet recognition of AOSD is often difficult due to its non-specific symptoms and overall rarity. Additionally, complicating the diagnosis of AOSD, the patient should meet Yamaguchi criteria but it is also considered a diagnosis of exclusion so other pathologies must be ruled out. AOSD can also be complicated by MAS (the form of HLH that occurs in AOSD is termed MAS). HLH/MAS is a potentially life threatening hyperinflammatory syndrome. HLH can present as a primary syndrome but is more frequently found as a secondary syndrome to infection, malignancy and inflammatory conditions such as lupus or AOSD. HLH/MAS is diagnosed by meeting 5/9 of HLH-04 criteria. Both AOSD and HLH/MAS can be treated with steroids and in severe cases, anakinra.
Conclusions: A high index of suspicion is needed to diagnose and treat AOSD and HLH/MAS. Appropriate evaluation of HLH includes workup for underlying cause such as infection, malignancy and inflammatory states such as AOSD.