Case Presentation:
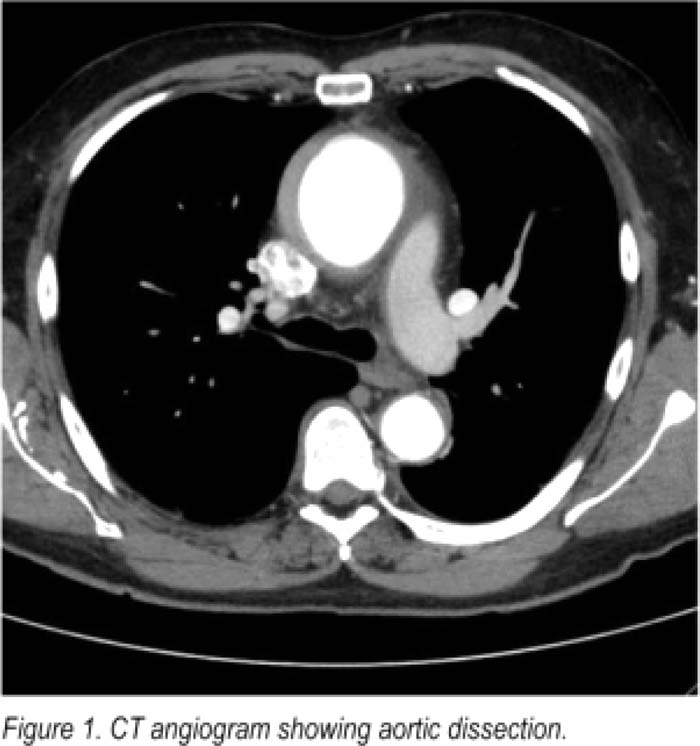
The patient is a 66‐year‐old man who was at work discussing a project with his colleagues when he had a sudden feeling of warmth and weakness come up from his legs toward his head He then felt lightheaded and passed out His coworkers activated EMS. EMS personnel noted a heart rate in the 30s, and the patient reported chest pressure and nausea. He was given aspirin, atropine, and nitroglycerin. Chest pressure was relieved. His past medical history included obstructive sleep apnea and newly diagnosed hypothyroidism. Patient never had chest pain or shortness of breath on exertion in the past. He reported being very active without any chest pain. He does not have any risk factors for coronary artery disease. Patient was admitted and ruled out for myocardial infarction. He underwent an exercise treadmill test next morning. During the stress test, he developed a similar chest pressure and had up to 1.5 mm of ST depressions in multiple leads. His chest pressure limiled his exercise, but it resolved with rest. Because of the positive stress test, he underwent cardiac catheterization the next day which did not show any significant coronary artery disease. Left ventricular function was normal. Cardiac catheterization was positive for mild to moderate aortic regurgitation and dilated aortic root, suggestive of chronic hypertension. A transthoracic echocardiogram was recommended to evaluate the aortic root dilatation and aortic valve insufficiency. Echocardiogram showed normal systolic function with ejection fraction in the range of 65% to 70%. Echocardiogram was positive for a dilated aortic root, mild aortic valve regurgitation, and a small pericardial effusion. Since these studies did not reveal the etiology of patient's chest pain and positive stress test, a CT angiogram of the chest was performed. CT scan showed ascending thoracic aortic aneurysm with intramural hematoma, concerning for impending dissection or rupture. Small pericardial effusion, likely hemopericardium, was aiso noted (Fig. 1). Patient successfully underwent emergency graft replacement of ascending aorta and with aortic valve resuspension. The patient was discharged from the hospital on day 8.
Discussion:
Other than syncope, this patient did not have any of the typical symptoms of aortic dissection. His blood pressure was not elevated. Chest x‐ray did not show widened mediastinum. There was no evidence of dissection on cardiac catheterization or transthoracic echocardiogram. Aortic dissection was finally diagnosed because it was still on Ihe list of differential diagnoses, and tests did not reveal The etiology of his symptoms.
Conclusions:
The purpose of this case presentation is to increase the awareness of the presentation of aortic dissection. Hospitalists should always consider aortic dissection in their differential diagnosis in patients presenting with chest pain despite atypical symptoms and presentations.
Author Disclosure:
C.‐H. Lee, none; J. Jahanmir, none.