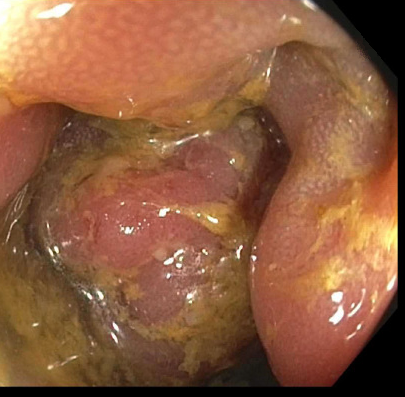
Case Presentation: A 27-year-old male with a history of HIV, well-controlled on HAART, presented with persistent hematochezia, rectal pain, and constipation for a month. His history was notable for unprotected anal receptive intercourse. Patient was reportedly seen at multiple other hospitals and received empiric treatments for gonorrhea, chlamydia & syphilis without relief. He was compliant with HAART with normal CD4 count (735) and undetectable viral load. On admission, CT scan noted severe mid-distal rectal wall thickening. On subsequent colonoscopy, a firm rectal mass with surrounding ulcerations concerning for malignancy was visualized. The biopsy result was negative for malignancy. The sample immunohistochemical stain was positive for CMV. However, given the tumor-like appearance and concern for inadequate sampling on previous biopsy, a repeat core biopsy was performed. This result showed colonic mucosa with hyperplastic features, which again was negative for dysplasia or malignancy. Patient was diagnosed with CMV colitis with associated pseudotumor. He was begun on valgancyclovir and after symptom improvement, he was discharged with a total three-week course with outpatient follow-up. On repeat evaluation with sigmoidoscopy six months later, resolution of the pseudotumor was noted.
Discussion: CMV is an opportunistic pathogen with high rates of infection in immunosuppressed patients. The most common area of involvement is the gastrointestinal tract with colitis being the most common manifestation. Pseudotumor formation is a rare occurrence in all CMV infections. Pseudotumor cases are rarely noted in literature and have been more frequently associated with severely immunosuppressed hosts, particularly those with AIDS. Kelesidis et al. describe a case of duodenal CMV associated pseudotumor with literature review listing 25 other similar reports. Of those, 14 reports are in HIV patients with 13 of those diagnosed with AIDS and 1 patient on zidovudine without specification of CD4 count or AIDS diagnosis. Another 11 reports were seen in patients without HIV though 5 of those 11 reports were seen in patients otherwise immunocompromised. Given the rarity of disease in an immunocompetent host, it can be easily misdiagnosed as colonic neoplasm or even polyp leading to a delay in treatment. Additionally, our patient was also found to have CMV colitis which has been associated with higher mortality. Galiatsatos et all in their meta-analysis of CMV colitis noted higher mortality particularly for the elderly, males, those with immune-modulating diseases, and those receiving surgical intervention.
Conclusions: Our case highlights the unique presentation of CMV infection and importance of maintaining a high index of suspicious essential for both timely diagnosis & management of CMV associated pseudotumor and colitis. This is critical to minimize the high risk of morbidity and mortality in these patients who are likely to be hospitalized given the severity of presenting illness.