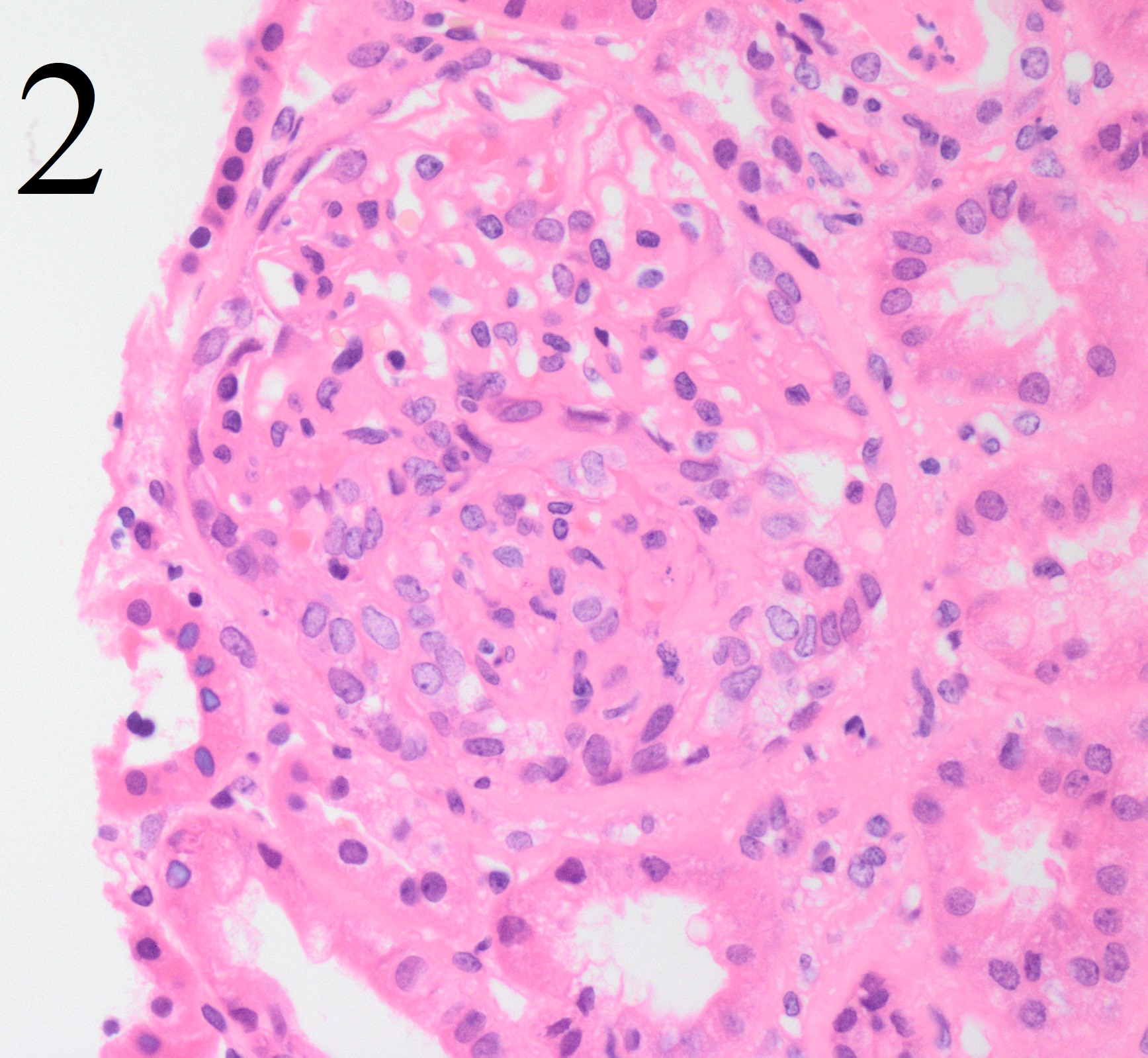
Case Presentation: A 25 year-old woman with severe persistent asthma, chronic self-resolving episodes of hemoptysis, history of miscarriage, and iron deficiency anemia secondary to heavy menses presented with sub-acute worsening shortness of breath and hemoptysis despite adherence to home inhalers. Patient had multiple prior hospitalizations requiring intubation for asthma exacerbations, complicated by hemoptysis. Upon presentation, she was found to be afebrile, normotensive, tachycardic to 130 bpm, tachypneic to 23, and saturating 95% on room air. Exam was notable for bilateral crackles at the lung bases. Labs were significant for microcytic anemia and UA with > 50 RBCs. EKG showed sinus rhythm. CTPA was negative for pulmonary embolism and demonstrated diffuse ground-glass opacifications with a new consolidation of the left lung (figure 1). She was started on CAP coverage and treatment for an asthma exacerbation. Given the findings of hematuria, an autoimmune workup was initiated, and she was found to have positive P-ANCA titers with normal IgE and complement levels, suggestive of vasculitis. She then underwent a renal biopsy demonstrating fibrocellular crescent glomeruli (figure 2) and immune complex deposits in the mesangium supporting the diagnosis of eosinophilic granulomatosis with polyangitis (EGPA). She was started on rituximab and steroid therapy and discharged home with plans for follow up with rheumatology and pulmonology.
Discussion: This case highlights several of the salient features of a patient with EGPA vasculitis. This disease process has been found to present in a sequential set of phases often beginning in the second to third decades of life, starting with a prodromal phase, followed by an eosinophilic phase, and finally a vasculitic phase. It has been established that these patients often initially develop asthma and allergic rhinitis during the prodromal phase, during which the classic laboratory markers of eosinophilia and ANCA positivity may be absent. In addition this phase of the disease can precede the vasculitis phase of disease by as much as ten years. In the eosinophilic phase, asthma symptoms are persistent and the patient develops peripheral eosinophilia. Finally, in the vasculitic phase, multi-organ damage often to the skin, lungs, heart, and kidneys occurs as a result of small and medium vessel involvement. Thus, for hospitalists who manage patients with asthma exacerbations, it is crucial to consider when an alternative diagnosis might be present. In this case, our patient presented with several symptoms and findings in her history that were incongruent with a simple asthma exacerbation. These symptoms include the history of recurrent hemoptysis, severe persistent respiratory symptoms despite medication compliance, and hematuria. The history of miscarriage should also have raised concern as there have been previous studies noting increased rates of miscarriage in patients with EGPA. At the time of presentation our patient would be classified in the vasculitis stage as evidence of necrotizing vasculitis had taken place.
Conclusions: EGPA is a systemic vasculitis that can affect multiple organs of the body; however, it is also a disease process that typically presents in a sequential set of phases that if not considered, can lead to a delay in diagnosis and treatment. For the hospitalist, this case highlights the importance of being mindful of and identifying risk factors of other disease processes, in this instance a vasculitis, that may present as a case of asthma exacerbation.