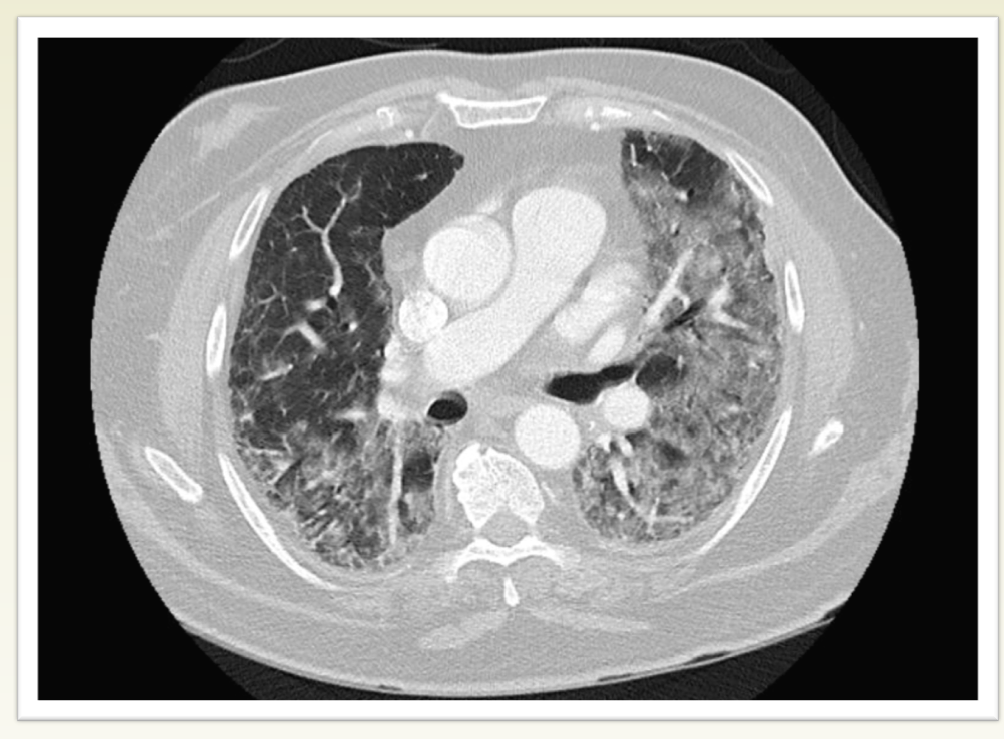
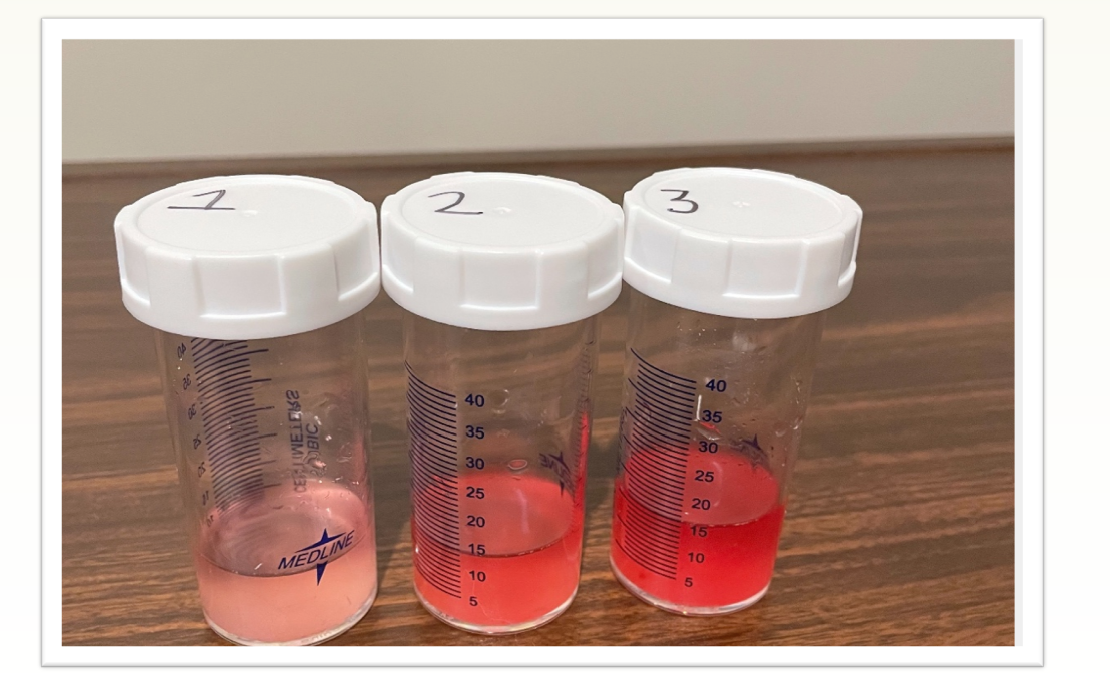
Case Presentation: 68 y.o. male presented with a purpuric rash, petechia, and suspected vasculitis. Past medical history included Hypertension, Non-Alcoholic Fatty Liver disease, Obstructive Sleep Apnea, Depression/Anxiety, DM type II and obesity. Significant presentations included pruritic rash and petechiae that started about a month before the presentation, worsening dyspnea, intermittent hemoptysis, and worsening bilateral pedal edema. Physical exam revealed palpable purpura on bilateral lower extremities extending up to the waist and upper extremities, unremarkable cardiopulmonary exams, and pitting edema of bilateral upper and lower extremities. CT scan of the chest showed bilateral ground glass opacities. Broncho Alveolar Lavage was performed, consistent with DAH. Urine microscopy was positive for hematuria and proteinuria. The patient was started on treatment with a pulse dose of Solumedrol 1gm daily x 3 days. A renal biopsy showed an exudative glomerulonephritis with IgA dominant mesangial deposits on Immune Florescence, consistent with IgA nephropathy/ HSP consistent with IgA nephropathy. Henöch- Schonlein purpura (HSP) was more likely in the setting of skin involvement. Skin biopsy was negative for lgG, lgG4, lgM, lgA, C3, fibrinogen inferring a lack of vasculitis lesion. However, the patient had already received a pulse dose steroid treatment before the biopsy. The patient’s respiratory status worsened and eventually required intubation. The patient was transferred to an outlying facility for further rheumatologic workup and continued tapered steroid dose. He improved clinically and was eventually extubated. The patient was ultimately discharged in stable condition to an acute rehab facility.
Discussion: Overt pulmonary involvement is rare in patients with IgA nephropathy/ IgA Vasculitis, especially in adults. Pulmonary capillaritis with IgA infiltration leading to necrosis and loss of capillary structural integrity is the most common pathophysiology behind DAH in IgA vasculitis. About 30-40% of patients with IgA nephropathy present with microscopic hematuria and mild proteinuria. Gross hematuria is more common in children and can delay a timely diagnosis in adults due to an insidious clinical course. Steroids are the mainstay of treatment with pulmonary involvement, with sterner adjunctive therapies, including plasmapheresis in severe cases. Prompt biopsy of skin lesions should be obtained as diagnostic yield significantly decreases after 24 to 48 hours of lesion onset. Also, initiation of corticosteroids before diagnostic intervention can obscure histopathologic findings. IgA nephropathy and HSP can be challenging to delineate when extra-renal manifestations are present. Further clinical studies are necessary to address these questions.
Conclusions: Diffuse Alveolar Hemorrhage (DAH) is a rare but life-threatening complication of IgA nephropathy/ IgA Vasculitis (Henoch-Schonlein Purpura). Here, we present an atypical clinical course of IgA nephropathy with predominant pulmonary symptoms. Renal and pulmonary findings can occur independently in IgA Nephropathy, which can lead to diagnostic ambiguity hindering appropriate and timely intervention, which could potentially be fatal. A high level of suspicion should be maintained in an appropriate clinical setting, due to high mortality and morbidity associated with the condition.