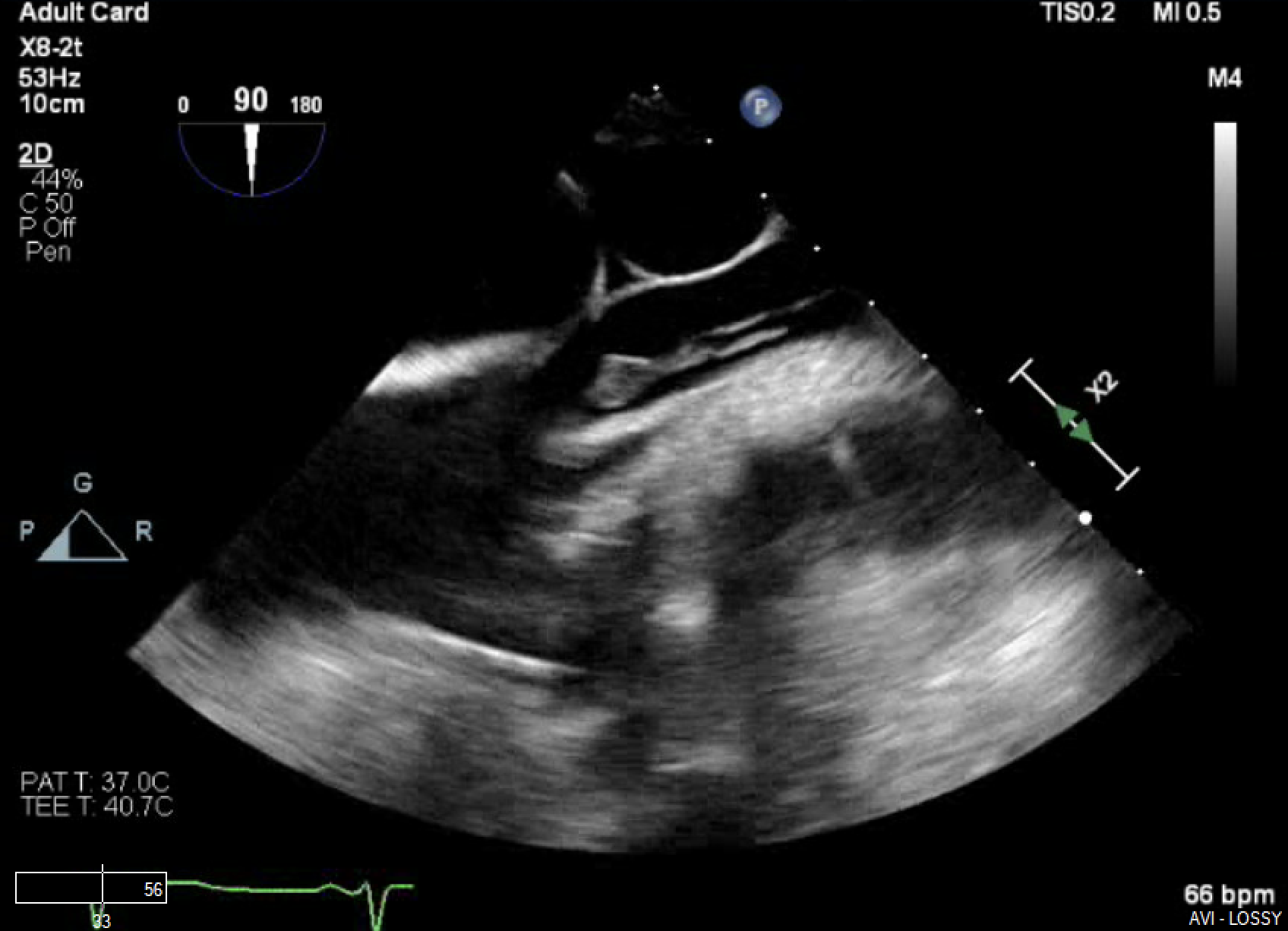
Case Presentation: A 45-year-old female with a history of agammaglobulinemia, gastroparesis post G & J tubes, complicated by failure to thrive necessitating TPN via a Hickman catheter presents, 2 years after catheter placement, with confusion, weakness and abdominal pain. She was admitted to the ICU for septic shock.Blood cultures were positive for MRSA and Candida albicans. Treatment with Vancomycin and Caspofungin was initiated. The Hickman catheter was removed and a TTE was performed, with no evidence of vegetations. Due to persistent bacteremia, a TEE was performed and identified a foreign body at the SVC – right atrium (RA) junction, determined to be a fibrin sheath with a mobile 1.1cm x 0.7cm vegetation at the tip (figure-1,2). A CT chest revealed bilateral pleural effusions and pulmonary septic emboli. Multidisciplinary options were discussed including vacuum thrombectomy, vascular stripping and conservative management. The decision was made to pursue antimicrobials and anticoagulation with unfractionated heparin (UFH). The team opted against intervention given the small sheath size, the likelihood of thromboembolism and the patient’s poor surgical candidacy due to severe malnutrition.Antibiotic recommendations included a 3-month Vancomycin IV course. The antifungal regimen transitioned from Caspofungin to Fluconazole. It was then switched to Isavuconazole due to QTC interval prolongation. On this regimen, the patient was found to have a pinpoint area of chorioretinitis. MRI of the brain and orbits demonstrated peripheral enhancements suspicious for septic emboli. Antifungals were transitioned to Amphotericin B for improved ocular and CNS penetration. A repeat TEE after 2 weeks of UFH infusion showed persistence of the fibrin sheath. The patient was bridged to Warfarin with a goal INR of 2-3. Three weeks after achieving sterile blood cultures on the medication regimen of Vancomycin IV, Amphotericin B and anticoagulation, the patient developed new fevers. She was found on repeat blood cultures to have MSSA. Repeat investigations including a 3rd TEE revealed persistence of the fibrin sheath, but resolution of the adherent vegetation.
Discussion: In a study by Tang et al [1], 11 patients were found to have infected fibrin sheaths identified by TEE. Eight of these patients had tunneled dialysis catheters. All had presented with bacteremia with gram positives. In all cases, the fibrin sheath was detected only by TEE, at the junction of the SVC and RA, with no evidence of valvular vegetations in any. Five patients were placed on anticoagulation with repeat surveillance. Thrombectomy was performed in 2. TEE clearance of the fibrin sheath was noted in 5 patients whom all survived. All-cause mortality was 36%. There are only sporadic reported cases of fibrin-sheath endocarditis [2-4]. Asymptomatic fibrin sheaths are reported in up to 47% of dialysis catheters [5]. There remain no guidelines for the management of such cases, but early recognition could be potentially lifesaving. Current treatment plans are based on prolonged antibiotic therapy and anticoagulation/thrombectomy. Fibrinolytic therapy is of limited utility due to the composition of the sheath.
Conclusions: Our case adds to the limited literature on this topic. This case is that of recurrent bacteremia and fungemia on an infected fibrin sheath. We based our management approach on findings of prior literature. For now, the best line of management is prevention through thoughtful catheter insertion and early removal.