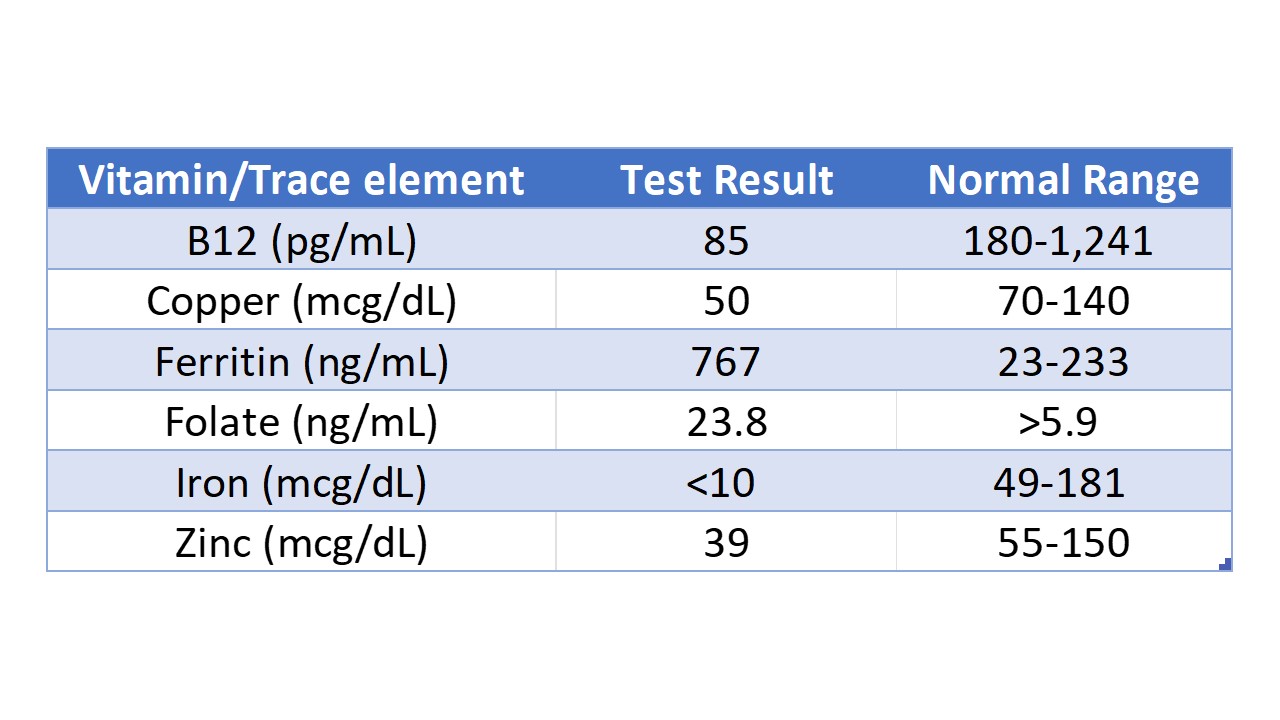
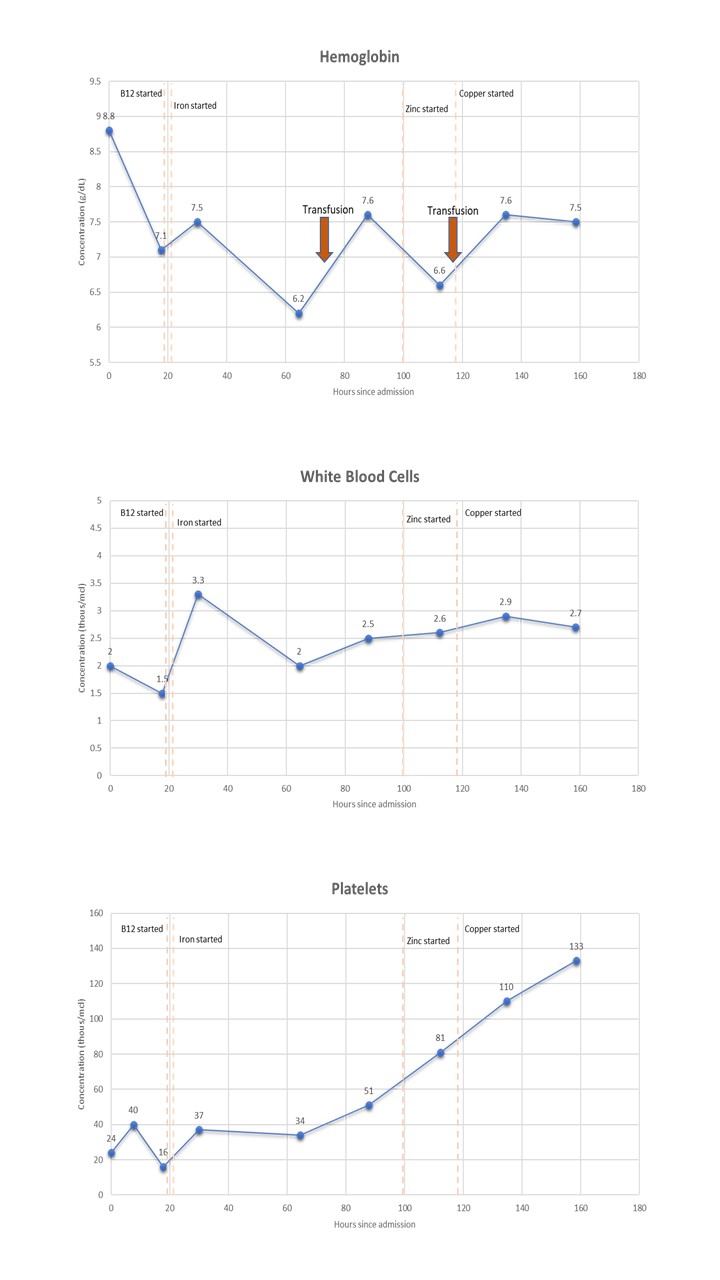
Case Presentation: A 55-year-old man with a history of chronic alcohol abuse, anxiety, and Crohn’s disease treated with right hemicolectomy and ileocolic anastomosis 30 years ago presented with symptoms of altered mental status, generalized weakness, and weight loss for 10 days. He endorsed chronic diarrhea but was not on immunosuppressants. He had a temperature of 100.1 F, blood pressure of 120/59 mmHg, pulse of 108 bpm, respiratory rate of 16 and saturating 93% on room air. He was found to have pancytopenia with a Hgb of 8.8 g/dL (baseline 15.8), WBC of 2.0 thous/mcL (baseline 4.6), platelet of 24.0 thous/mcL (baseline 170-200), and MCV 135.1 fL. Iron panel indicated anemia of chronic disease and iron deficiency; Vitamin B12 was low. Given his neurological and hematological findings, the patient’s pancytopenia was suspected to be due to vitamin B12 deficiency secondary to chronic alcohol use. He initially received vitamin B12 and iron supplementation. While his neurological function improved, his pancytopenia persisted, requiring 2 units of packed red blood cell transfusion. Further workup revealed copper deficiency, which was suspected to be due to malabsorption in the setting of Crohn’s disease and poor oral intake. Copper supplementation was initiated at 0.4mg IV daily, after which his pancytopenia began to improve. The patient was discharged on vitamin B12 1000mcg injection once weekly and oral copper 2mg once daily.
Discussion: Copper deficiency, a rare but significant condition, can lead to a range of hematologic and neurologic manifestations due to its crucial role in biochemical processes [1-2]. Its deficiency is often indistinguishable from subacute combined degeneration due to cobalamin deficiency, or cytopenias due to myelodysplastic syndrome [1, 3-5]. Gastrointestinal surgeries account for almost half of the cases of acquired copper deficiency [6-9]. Malabsorption due to conditions such as celiac disease, inflammatory bowel disease (IBD), bacterial overgrowth, and cystic fibrosis have been linked to cases of copper deficiency [10-15]. While most adults and children with Crohn’s disease are not copper deficient, increased losses are observed in those with profuse diarrhea, high-output fistulas or ostomies, or those maintained on parenteral nutrition without mineral supplements [13, 16]. Hematologic manifestations of copper deficiency most commonly present as anemia, followed by neutropenia, and thrombocytopenia [1]. Neurological manifestations include weakness, numbness, paresthesia, pain, or absent reflexes [2]. The management of copper deficiency depends on the severity of anemia and the underlying mechanism [17]. The copper deficit is readily corrected with parenteral or oral copper preparations that provide 2 mg of elemental copper per day, and the hematologic abnormalities return to normal in less than two months [18-22].
Conclusions: Clinical copper deficiency is a rare but increasingly recognized cause of anemia, neutropenia, and bone marrow dysplasia. In patients with iron and B12 treatment-resistant pancytopenia with concurrent neurological abnormalities, copper deficiency should be included as a part of the differential – particularly in patients with risk factors for malabsorption. A thorough evaluation includes comprehensive hematologic workup and measurement of copper-related markers. Appropriate copper supplementation can lead to successful management and resolution of associated symptoms.