Case Presentation:
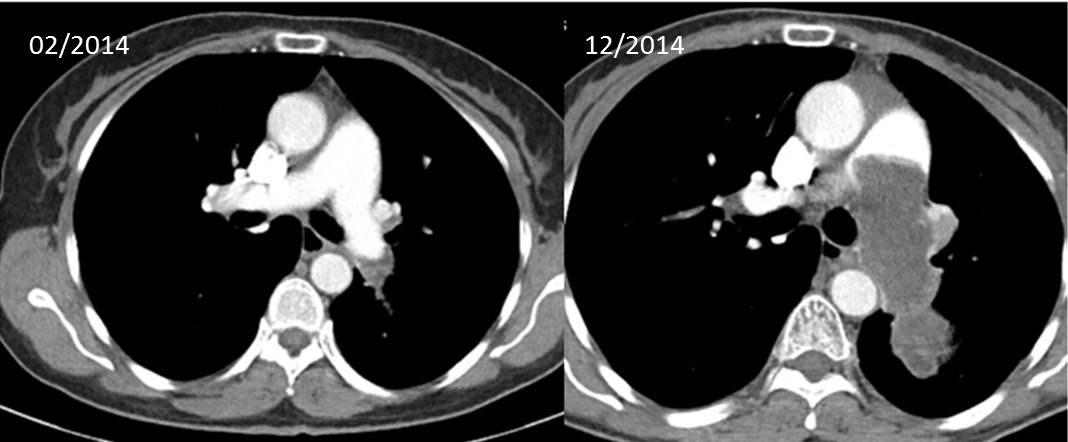
A 59yo woman with past medical history of Diabetes Mellitus, Hypertension and hyperlipidemia presented to her primary care physician with a 2 week history of acute onset left sided chest pain and difficulty with deep inspiration. Chest X-ray was suggestive of atypical infection; she completed a course of oral antibiotics, but symptoms and X-ray findings persisted. CT Thorax with contrast reported an acute thrombus in the left lower pulmonary artery. She was hospitalized immediately, started on heparin and later completed 6 months of warfarin. Shortly after, a paroxysmal cough developed and repeat CT revealed a filling defect occupying the entire left main pulmonary artery extending into the main pulmonary artery, consistent with a tumor thrombus. FDG positron emission tomography demonstrated avidity of the tumor thrombus, felt to represent primary angiosarcoma. Core needle biopsy revealed poorly differentiated high-grade pleomorphic sarcoma, consistent with intimal sarcoma versus undifferentiated sarcoma. The tumor was determined to be unresectable and 13 months after initial onset of symptoms, she started palliative chemotherapy (docetaxel/gemcitabine and later pazopanib).
Discussion:
Sarcomas are the most common primary tumors of the pulmonary arteries, yet they are rare and difficult to diagnose. PAS is usually asymptomatic until there is significant vessel occlusion and presents with symptoms like dyspnea, chest pain and cough. On conventional chest X-ray PAS usually manifests as hilar, mediastinal, or pulmonary artery enlargement (53%), pulmonary nodule (40%), cardiomegaly(33%), and diminished pulmonary vascularity(18%). CT pulmonary angiography is good at detecting intravascular processes but it is difficult to differentiate tumor from thromboemboli, further studies are needed.
The mainstay of therapy is radical surgical resection and neoadjuvant chemotherapy if possible. However because the tumor usually involves vital cardiac structures surgical resection can be challenging. Also initial misdiagnosis and acute cardiorespiratory symptoms requiring urgent surgery sometimes preclude neoadjuvant chemotherapy. Patients undergoing an attempt at curative resection have a median survival of 36.5 months compared with 11 months for those undergoing incomplete resection. Median survival is also better for patients undergoing surgery/chemotherapy/radiation (survival of 5-7 years has been reported), compared with those on single therapy.
Conclusions:
The diagnosis of PAS represents a challenge for physicians and early diagnosis is of the utmost importance due to the poor prognosis and high mortality associated with it. The symptoms and imaging are often misleading. In patients suspected of having a pulmonary embolism who do not respond to initial anticoagulation, physicians should consider further investigation with gadolinium-enhanced magnetic resonance imaging or FDG-PET.