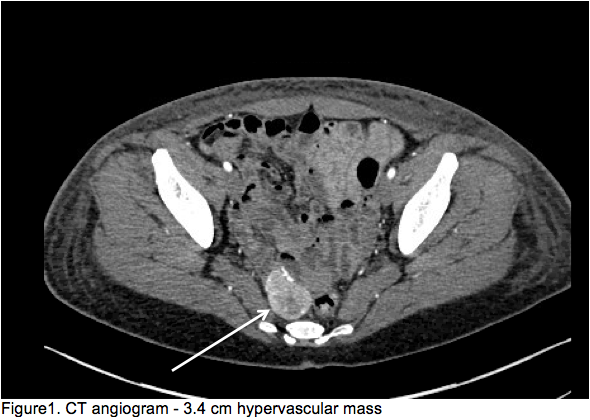
Case Presentation: 51 year old female with past medical history notable only for recent knee pain with intermittent NSAID use presented with melenic stools and one episode of coffee ground emesis.On presentation she was tachycardic and hypotensive with initial hemoglobin of 4.9 (units) with improvement in vital signs post blood transfusion. Initial CT abdomen/pelvis without contrast performed in the emergency department revealed only a heterogeneously enhancing left adnexal mass. Small bowel enteroscopy was pursued without source of bleeding identified. Colonoscopy showed multiple diverticula in the sigmoid colon, and non-bleeding external and internal hemorrhoids, blood was found throughout the colon without an identifiable source. CT angiogram showed a 2.5 x 3.2 cm lesion in the tributary of the SMA consistent with possible vascular, small bowel, left ovarian etiology. This resulted in gynecology consultation for further investigation with pelvic ultrasound showing a 3.4 cm solid hypervascular mass on left side of cul de sac likely involving pelvic bowel loops and multiple fibroids. CEA and CA125 were within normal limits. Colorectal surgery was consulted for surgical resection as this mass was felt to be the culprit lesion and the patient had continued gastrointestinal bleeding causing her to be transfusion dependent. Repeat CT angiogram again showed a 3.4 cm hypervascular mass with vascular supply from the SMA (Figure 1). A diagnostic laparoscopy with small bowel resection with primary anastomosis was performed. Surgical pathology revealed a benign gastrointestinal stromal tumor, 4 cm in greatest dimension with negative margins.Post-operatively, the patient clinically improved and did not require further blood transfusions.
Discussion: Gastrointestinal stromal tumors (GIST) are mesenchymal tumors of the gastrointestinal tract arising from smooth muscle pacemaker interstitial cell of Cajal, a majority being positive for CD 117, others may express PDGFRA and BRAF in addition to KIT.GISTs most often arise in the stomach (60%–70%) and small intestine (25%–30%), but less frequently occur in the colorectum (5%–15%), duodenum (5%), and esophagus (< 2%).They often grow relatively slowly and present with nonspecific symptoms and consequentially are often found incidentally, but can present with spontaneous perforation or hemorrhage. GISTs are often found using appropriate imaging modalities such as CT scan or MRI of the abdomen, however do not have characteristic radiographic features that can definitively diagnose them, making diagnosis difficult. The primary treatment remains surgical excision with imatinib as adjuvant therapy in cases of intermediate to high-risk tumors, metastatic disease or non-operable candidates. This case required multiple imaging and additional consultations to demonstrate the hypervascular lesion as the culprit given negative endoscopic examinations that may have delayed surgical resection and required continued transfusions.
Conclusions: Our case shows that a high index of suspicion is required to make the appropriate diagnosis of GIST in the small bowel.