Background: Like many institutions nationwide, our health system, an urban tertiary care academic medical center, has experienced challenges due strained hospital capacity. Hospitalists frequently face feedback to place discharge orders as early as possible in the day, for reasons as diverse as assisting patients with obtaining a ride home to expediting bed turnover for the next admission. However, fitting discharges into the rounding structure of a busy morning as a direct care hospitalist is a challenging puzzle, as many discharges take thoughtful planning, multidisciplinary discussions, and close attention to detail. As a result, despite attempts to increase accuracy of estimated date of discharge (EDD) and advance time of discharge, average discharge order time, and rates of accurate EDD these remain constant problems in our institution.
Purpose: We sought to create a systematic approach to day-of-discharge communication, currently leveraged by our direct care hospitalist Clinical Assistant, to jumpstart the discharge process for select patients.
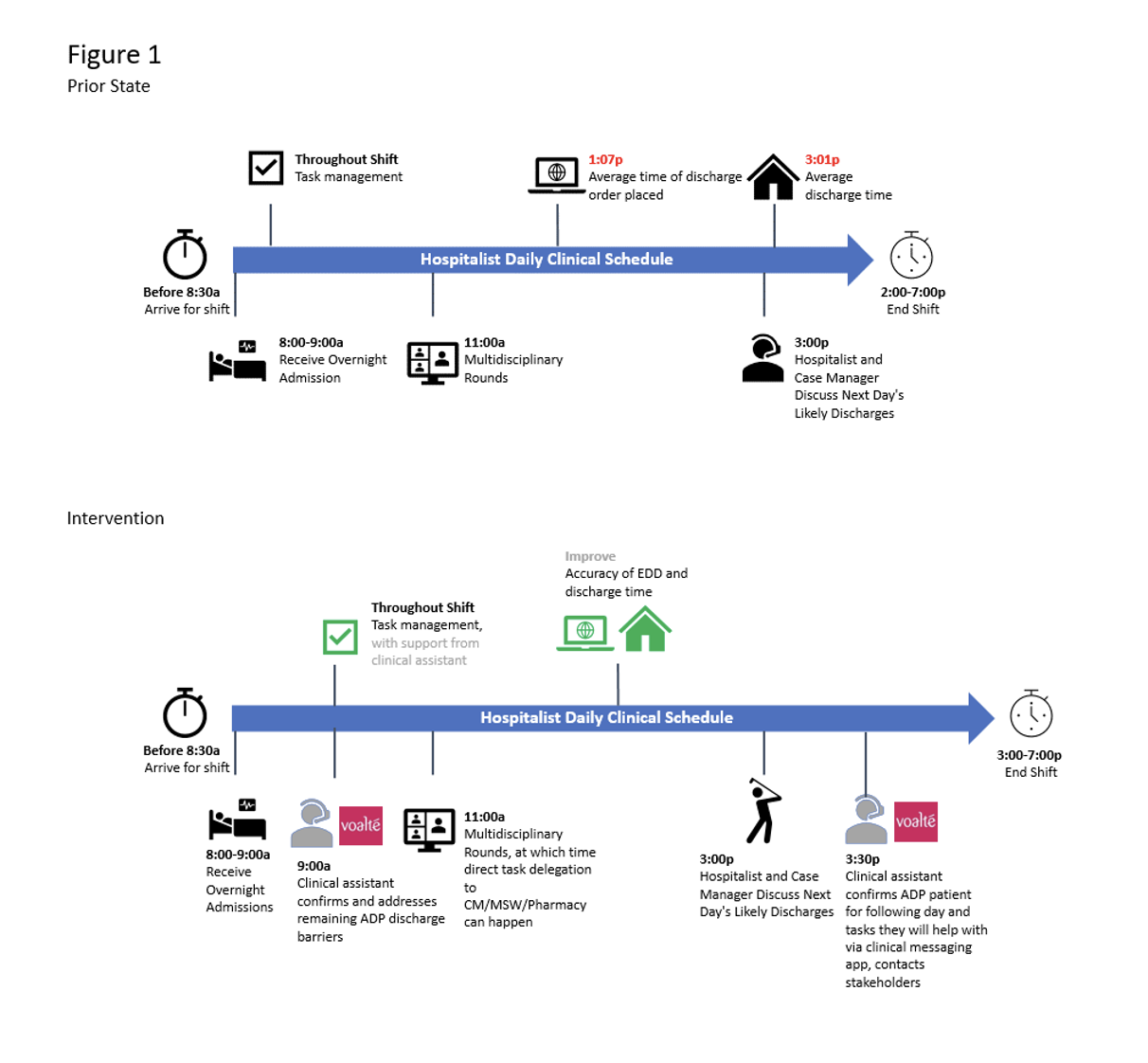
Description: We engaged with multiple stakeholders including pharmacy services, nursing staff, nursing leadership, unit leadership, and the direct care hospitalist service leadership to gather input and ideas for improvement. We also presented the idea at our hospitalist division’s Quality Improvement Committee and to our division at large for more input. After mapping out the current state, we outlined common tasks that the direct care Clinical Assistant could address and a general approach to each. The core aspects of the pilot communication protocol are displayed in Figure 1. We also designed a careful data tracking process to measure engagement with the program, and how common each type of task was for the Clinical Assistant. Additionally, we created a plan for following up on our division’s goal to improve EDD accuracy and the health system’s goal of reduction in length of stay. Our pilot’s preliminary data collection began in October 2023.
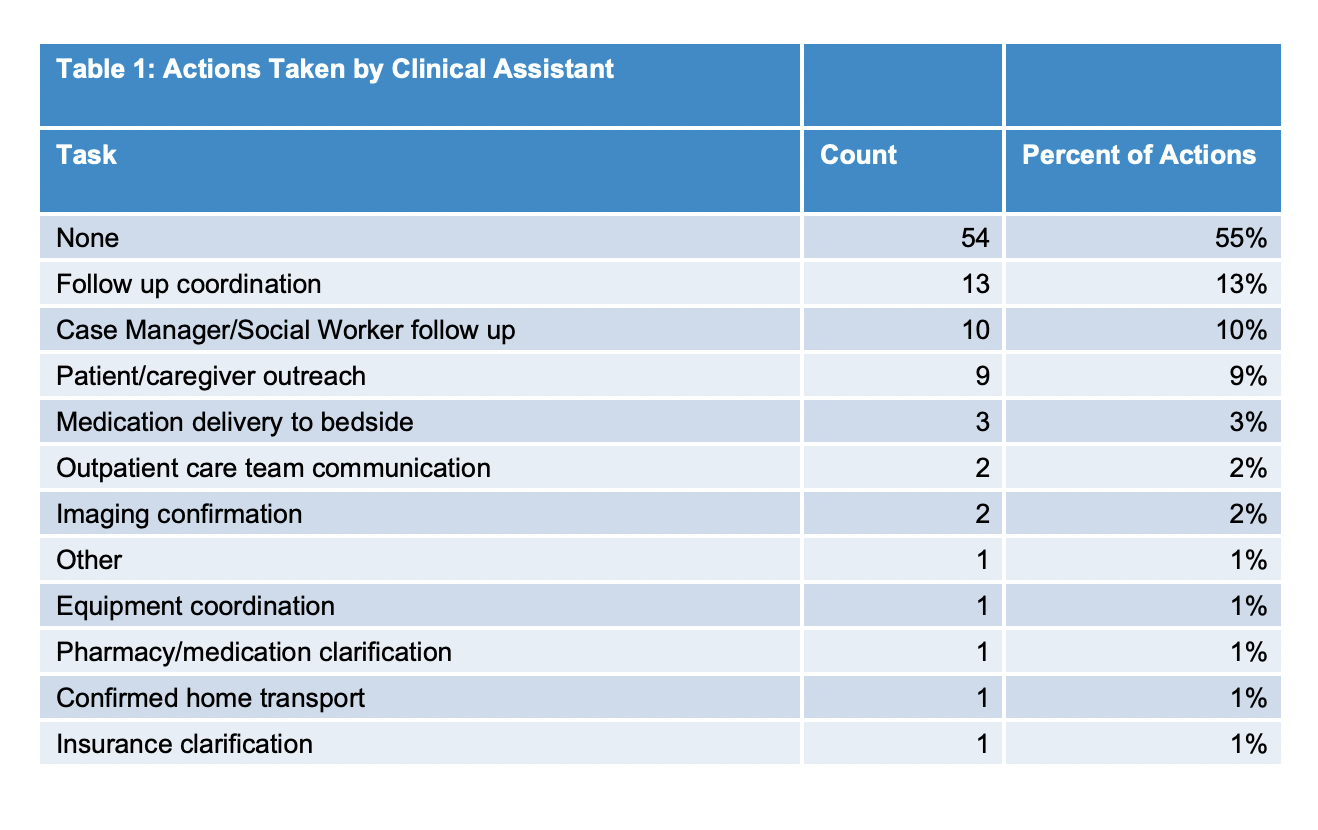
Conclusions: Over the course of the pilot month the Clinical Assistant initiated contact with 9 direct care hospitalists daily Monday through Thursday, and garnered a response rate of 58% to the initial question of which patient was likeliest to discharge the following day. In 45% of instances, the Clinical Assistant was able to assist with a task that the hospitalist identified as relevant to the patient’s readiness for discharge (Table 1). In all patients who were identified for ADP, the average discharge order time by the hospitalist improved by ~25 minutes compared to non-ADP patients. However, there was minimal difference in the average physical discharge time between the two groups, which will require additional efforts toward workflow improvement with our patient-facing colleagues (RN staff and leadership).