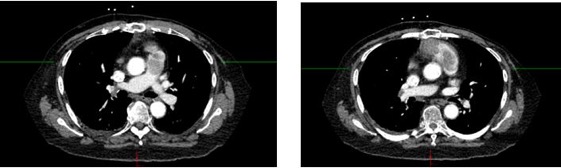
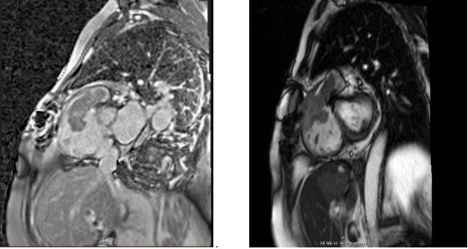
Case Presentation: An 80-year-old female with a past medical history of breast cancer status post bilateral mastectomy and hepatocellular carcinoma status post radiation therapy presented with chest pain and progressive shortness of breath. The Computed tomography (CT) chest revealed a mass in the right ventricle extending into the main pulmonary artery with flattening of the interventricular septum suggestive of right ventricular strain, concerning a sub-massive PE (Image 1). An Abdominal CT showed multiple hypodense liver lesions suggesting disease progression of hepatocellular carcinoma. Doppler ultrasonography of bilateral upper and lower extremities showed no evidence of venous thrombosis.The patient was started on the heparin drip and underwent a suction thrombectomy by interventional radiology. The procedure was unsuccessful due to the rigidity of the clot and complications from blood loss and hence was aborted. An echocardiograph showed a large heterogenous mass within the right ventricle (RV) with partial outflow obstruction of the RV outflow tract (RVOT). A cardiac magnetic resonance imaging showed a highly vascular and heterogeneous mass in the RV and RVOT concerning for malignancy. (Image 2). Subsequently, the biopsy result from the thrombectomy sample confirmed the mass as metastatic hepatocellular carcinoma. Oncology was consulted, and the patient was offered palliative chemotherapy based on the immunohistochemistry of the tumor cells, however, the patient chose palliative care.
Discussion: Pulmonary embolism (PE) is a condition caused by blockage of pulmonary vasculature by clumps of material. Most PE cases are caused by venous thromboembolism ( VTE), but this is not always the case. PE can be caused by tumors, fat, air, amniotic fluid, foreign bodies, insects, septic materials, etc (1). Tumor embolism (TE) occurs when solid tumors seed the systemic circulation with individual cells, clusters of cells, or large tumor fragments causing microvascular obstruction, mimicking VTE as in our case. A TE misdiagnosed as a sub-massive or massive VTE could have serious clinical implications as administering systemic thrombolytics or performing suction thrombectomy in these cases could result in catastrophic outcomes such as hemorrhage. In many instances, a tissue sample is not feasible, and the diagnosis relies solely on clinical suspicion and radiographical findings.
Conclusions: The incidence of tumor embolism (TE ) is estimated by an autopsy series to be 3% to 26% in patients with solid tumors(2). The most common cancers associated with TE are gastric carcinoma, breast carcinoma, pulmonary carcinoma, renal cell carcinoma, and hepatocellular carcinoma (2). Diagnosing tumor embolisms could be challenging as they tend to mimic VTE with similar radiological and clinical characteristics. It is important to have a high index of suspicion and broad differential in patients with a history of carcinoma as misdiagnosed cases could result in catastrophic complications and missed opportunities for treatment.