Case Presentation: A 41-year-old man presented with months of a dry cough, non-bloody diarrhea, and an unintentional 20-lb weight loss, as well as one day of a severe headache. His history was notable for injection drug use, homelessness, and HIV infection for which he was not taking any medications.
Initial vitals were temperature 38.3°C, blood pressure 129/79, heart rate 100 beats per minute, and oxygen saturation 97% on room air. He had oropharyngeal exudates, decreased basilar breath sounds, and a normal neurologic exam without nuchal rigidity. His absolute CD4 count was 18 x106 cells/L, and HIV viral load was 71,550 copies/mL. LP revealed an elevated opening pressure; CSF gram stain showed rare yeast and culture grew numerous Cryptococcus neoformans.
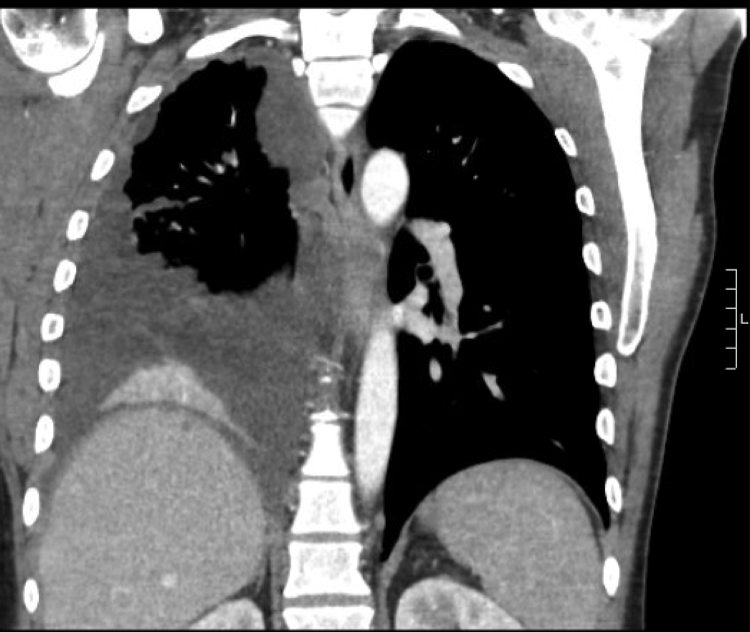
A chest CT showed a right pleural effusion associated with extensive pleural nodularity and mediastinal lymphadenopathy that were concerning for malignancy (Figure 1). A positron emission tomography-computed tomography (PET-CT) scan was non-diagnostic due to equipment failure. A thoracentesis revealed clear, serous, and exudative pleural fluid, and the acid-fast bacilli culture, Mycobacterium tuberculosis complex PCR, and cytology were all negative on two separate days. Bacterial and fungal cultures of the fluid ultimately grew C. neoformans.
The patient was treated with liposomal amphotericin B and flucytosine. He left against medical advice prior to induction completion.
Discussion: Our institution cares for a high volume of HIV-infected and immunocompromised patients, and this was the first time this organism has been isolated from pleural fluid in more than five years. Pulmonary manifestations are seen in <50% of patients presenting with cryptococcal meningitis, but pleural effusions are only observed among 5% of patients with lung disease. Pulmonary cryptococcosis more commonly presents as interstitial infiltrates (76% of pulmonary cases), occasionally with mediastinal or hilar adenopathy (11%) or pulmonary nodules (5%).
Appropriate management of pulmonary cryptococcosis requires evaluation for disseminated disease, including a lumbar puncture to rule out CNS involvement even in the absence of symptoms. While isolated pulmonary cryptococcosis can be treated with fluconazole alone, CNS and disseminated disease are treated with an induction phase of amphotericin and flucytosine followed by a consolidation phase and maintenance therapy with fluconazole monotherapy. The utilities of chest tube placement to drain cryptococcal pleural effusions, serial imaging, and documentation of pleural fluid culture sterilization have not been well studied and remain uncertain.
Conclusions: Culture-positive pleural effusions are a rare manifestation of disseminated cryptococcal disease in patients with advanced HIV. Hospitalists should recognize that pulmonary manifestations may be non-specific and mimic malignancy. This case highlights the importance of including pulmonary cryptococcosis in the differential diagnosis of a unilateral pleural effusion in a patient with advanced HIV and cryptococcal meningitis.