Case Presentation: A 76- year old smoker woman with a medical history of emphysema and left MCA stroke six months back, presented with acute bilateral occipital headache and visual impairment.On Exam, she was well appearing, normal vital signs, and no murmurs on heart exam. Neurological exam was normal except for dysmetria due to visual impairment (cortical blindness). The rest of her exam was unremarkable.
Initial labs were remarkable for WBC 16.3 K/uL, Plt 61 K/uL and LDH 725 U/L.
Brain MRI showed new bilateral PCA territory ischemic stroke. She had schistocytes on peripheral smear. Hence, she was started on Plasmapheresis for presumed TTP while awaiting the ADAMTS13 result. She did have consolidation in her left lung on CXR and was started on antibiotics for presumed pneumonia.
ADAMTS13 and antiphospholipid syndrome workup returned normal. Transthoracic echocardiogram revealed a large mitral valve vegetation 2.2 cm, so first blood culture was sent and Broad spectrum antibiotics started for possible infectious endocarditis (IE).
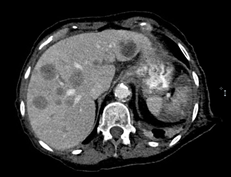
Abdominal Ultrasound for abdominal pain showed numerous hepatic lesions consistent with metastatic disease, confirmed by CT scan. CT scan of her chest revealed 1.5 cm spiculated nodule in the left upper lobe.
Liver biopsy was positive for moderately differentiated adenocarcinoma. Immunoprofile suggested lung origin.
Blood culture did not grow any organism. She was discharged to a nursing facility to complete her antibiotic course and follow up with her oncologist.
One week later, she presented again with acute encephalopathy. Brain MRI showed new scattered strokes within the right MCA and left ACA territories. Goal of care discussion with her family resulted in focusing on comfort care.
Discussion: Endocarditis is a common disease in the acute care setting. In this case, IE was possible based on the modified Duke Criteria. The malignancy along with negative blood culture made Nonbacterial Thrombotic Endocarditis (NBTE) very plausible diagnosis as well. The most important factor in the formation of these valvular vegetations is the hypercoagulable state associated with malignancies. Systemic emboli occur in nearly 50% of patients with NBTE and usually result in the presenting symptom.
Echocardiographically, NBTE vegetations are indistinguishable from those of IE but histologically, they are characterized by an amorphous mixture of platelets, fibrin, and red blood cells without microorganisms or inflammation. Conversely, inflammatory cells are strongly involved in the pathogenesis of IE. PET scan has been proposed to help with the differential diagnosis. The usual treatment of NBTE is anticoagulation. Contrarily, anticoagulation is potentially hazardous in infective endocarditis, with a substantial risk of intracerebral hemorrhage.
Conclusions: Stokes in different territories imply cardioembolic phenomenon. When considering endocarditis as an etiology, it is imperative to obtain blood culture before starting antibiotics. Early differentiation of IE from NBTE is crucial due to completely different treatment plans. NBTE should be strongly considered in cases of culture-negative IE when no clinical improvement on the appropriate antibiotics, and in a cancer patient who develops any embolic event such as ischemic stroke.
.jpg)