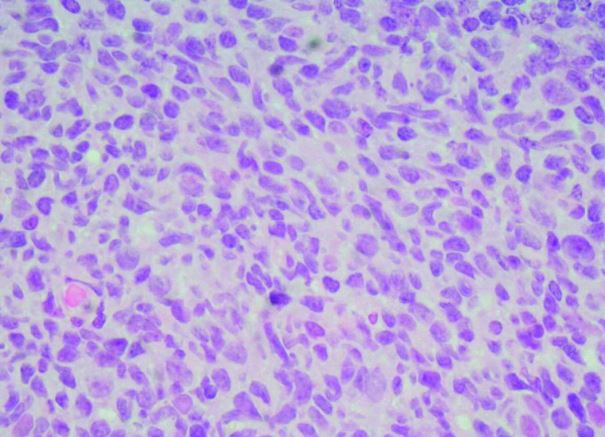
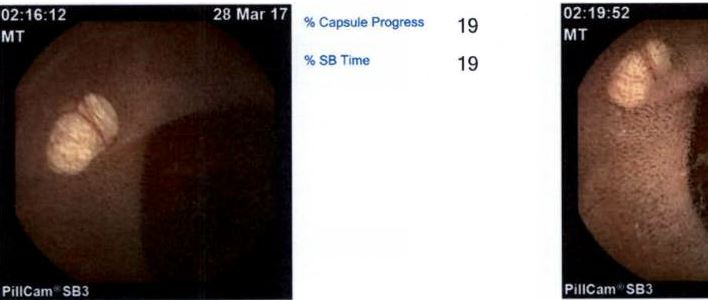
Case Presentation: A 73-year-old female with PMH of iron deficiency anemia, laparoscopic cholecystectomy, and hernia repair had received iron transfusions as well as blood transfusion. Despite which, her hemoglobin remained low, 7.3gm/dl. She was fatigued, but denied abdominal pain, black stool, vomiting blood, fevers or chills. She had an upper endoscopy that was unremarkable as well as colonoscopy that showed one benign polyp. She also had two episodes of small bowel obstruction in a month period that resolved spontaneously. CT scan was done due to small bowel obstruction to rule out any neoplastic process that could be causing the anemia. It showed acute on chronic distal ileitis as well as some residual inflammatory changes in the small bowel mesentery. She was discharged but readmitted in 3 days with third episode of bowel obstruction. Hemoglobin was 11.9gm/dL, WBC 4.3, electrolytes were normal, Creatinine was 0.59. Repeated upper endoscopy and colonoscopy were normal. Capsule endoscopy showed capsule did not reach Cecum, but a few small lymphangiectasias were seen in the jejunum and a large crater ulceration was seen in the ileum, but no obvious tumor, but the small bowel distal to this was not seen. Decision was made she will need surgical exploration given these findings. She finally underwent exploratory laparoscopy that converted to a mini-abdominal laparotomy with lysis of adhesions, small bowel resection with functional end-to-end anastomosis. Small bowel pathology showed lymphoid proliferation with follicular differentiation. Flow Cytometry showed CD19 positive cells constitute 2% of total cells and demonstrate polytypic light chain expression. CD3 positive T-cell represented 15% of total cells. She was started on induction Rituxan therapy with good response. Repeated imaging studies showed stable disease.
Discussion: Gastrointestinal follicular lymphoma is a variant of follicular lymphoma. The GI tract is commonly involved extra-nodal site for non-Hodgkin lymphomas. These tumors form a highly heterogeneous group, with high-grade lymphomas and mucosa-associated lymphoid tissue (MALT) lymphomas being the most common subtypes. Follicular lymphoma of the GI tract (GI-FL) is relatively rare, accounting for only 3.6% of GI non-Hodgkin lymphomas. Many of these cases are diagnosed incidentally. Due to its rarity, there is no established guidelines on the optimal diagnostic strategy for patients with primary gastrointestinal follicular lymphoma or secondary gastrointestinal involvement of systemic follicular lymphoma. It is challenging to confirm the diagnosis, but Gastroenterologist may try various modalities for diagnosis including endoscopy, colonoscopy, double lumen enteroscopy and capsule endoscopy.
Conclusions: Primary gastrointestinal follicular lymphomas make up 1%–3.6% of all non-Hodgkin lymphomas. Patients may present with abdominal pain and bleeding, but most cases are incidentally diagnosed on endoscopy. Evaluation of the entire small bowel tract is important. This case highlights the endoscopic findings that led to the diagnosis of this rare disease and the role for close clinical monitoring as a treatment strategy in this rare disease process.