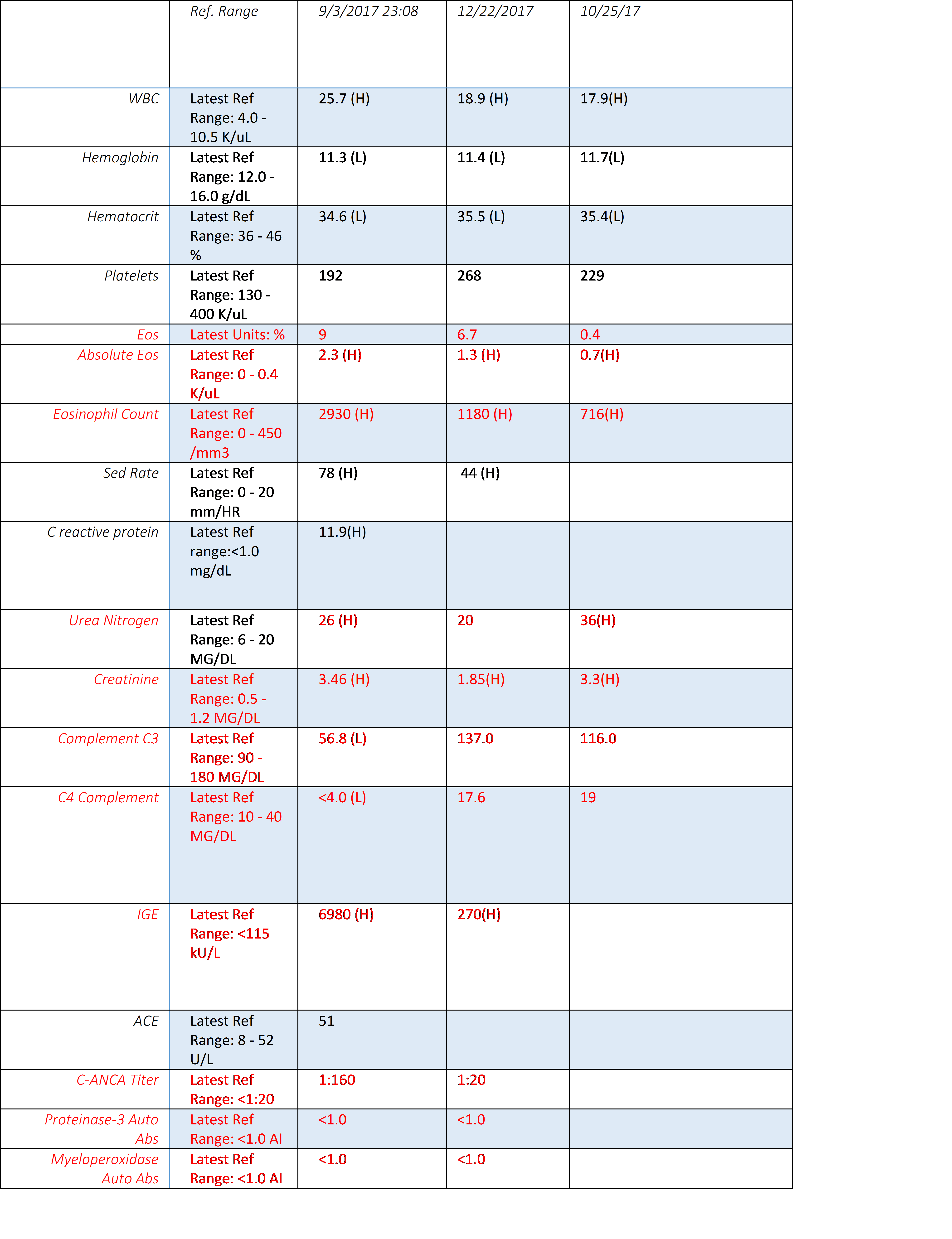
Case Presentation: A 45-year-old woman presented to Emergency Department (ED) with a 1-weeks history of a sore throat, sinus congestion and dry cough. She was diagnosed with an upper respiratory tract infection and treated with amoxicillin/clavulanic acid. After 3 doses, she developed a high-grade fever and pink confluent pruritic maculopapular rash on arms and legs that progressed to her entire body. She returned to the ED and was diagnosed with a drug induced rash. She was treated with prednisone and the antibiotic was stopped. She returned to the ED with worsening rash, fever and hypotension. Her physical examination confirmed bilateral lower zone pulmonary crackles. Her laboratory tests showed leukocytosis, eosinophilia, acute kidney injury and lactic acidemia (Table 1). Computerized tomography scan confirmed diffuse lymphadenopathy, mild lung base consolidations and paranasal sinusitis. She was admitted for septic shock and treated with broad spectrum antibiotics. A skin rash biopsy confirmed leukocytoclastic vasculitis and a lymph node biopsy showed atypical lymphocytic proliferation and excluded malignancy. Infectious disease, Rheumatology, and Nephrology were consulted and entertained a diagnosis of Epstein–Barr virus (EBV) infection. She was treated pulse dose steroids, followed by high dose oral steroids, and she discharged on steroid taper with outpatient follow up. Drug reaction with eosinophilia and systemic symptoms (DRESS) is excluded as symptom onset was immediate rather than delayed. Renal biopsy performed during the hospitalization resulted after her discharge and showed eosinophilic interstitial inflammatory infiltrates.She had two further hospitalizations with similar symptoms that again responded to steroids. Hematology was consulted and a bone marrow biopsy excluded malignancy. Churg-Strauss syndrome is ruled out given the absence of necrotizing granulomatous vasculitis in skin or renal biopsy and negative PR3, MPO antibodies. A diagnosis of Hypereosinophilic Syndrome (HES) was made. She was treated with azathioprine on her last admission and has had no further hospitalizations. She is currently being treated outpatient with Benralizumab (Fasenra).
Discussion: Hypereosinophilic syndrome (HES) can be peripheral hypereosinophilia (HE) or tissue HE that is associated with HE-related organ damage. Peripheral HE is defined as an elevated absolute eosinophil count (AEC) >1.5 x 109 /L on two occasions more than 1 month apart. Tissue HE is defined bone marrow eosinophils greater than 20% and/or tissue infiltration by eosinophils or deposition of eosinophil granule proteins. Reactive or secondary HE is associated with allergies, infections, autoimmune and neoplasms disease and needs to be excluded to make a diagnosis of primary HES.High dose steroids is the first line therapy for acute HES and in steroid responsive patients, the AEC decreases within 24 hours. Steroid sparing agents including hydroxyurea, imatinib, cyclophosphamide, azathioprine, rituximab and methotrexate can be considered depending on the subtype of HES. Recently several biologic/monoclonal Ab treatments are available and are promising for people with HES.
Conclusions: HES is associated with wide spectrum of organ dysfunction and hence evaluation of patients with HES requires complex testing and multidisciplinary approach. Early suspicion for and recognition of HES is crucial for hospitalists as involvement of subspecialists is essential in the management of HES and prevents readmission.