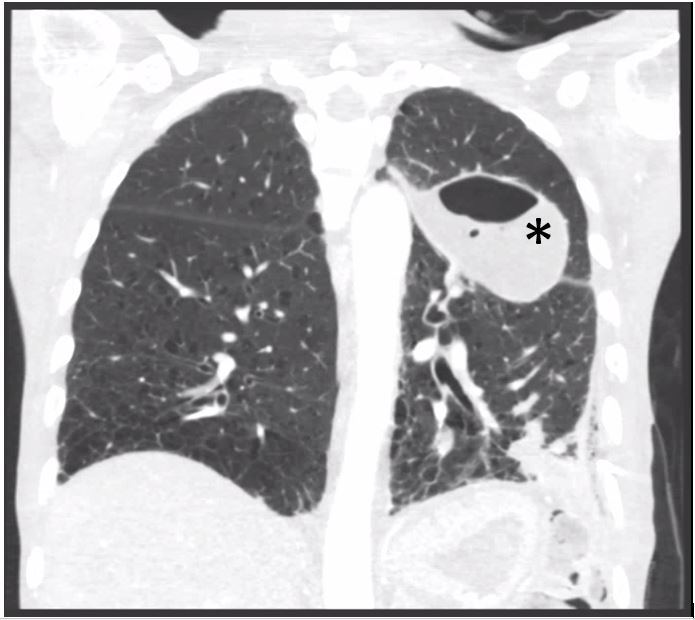
Case Presentation: A 66-year-old man with uncontrolled type 2 diabetes mellitus (hemoglobin A1c = 18.1%) presented with one month of worsening pleuritic chest pain, productive cough and 10-pound weight loss. He denied any gastrointestinal (GI) symptoms, including diarrhea or abdominal pain. He worked as a clinical nursing assistant. Patient denied any recent international travel, animal exposures or raw food ingestion. His medications included insulin glargine, sliding scale insulin, metformin, aspirin, atorvastatin and lisinopril. Vital signs were notable for respiratory rate of 18 to 22 and oxygen saturation greater than 95% on room air. On examination, he appeared cachectic with temporal wasting. Breath sounds were markedly decreased in the left lower and middle lobes of his lung. Abdomen was benign. Laboratory studies revealed a white blood cell count of 16,900/mm^3 with 30% bandemia and a lactate of 3.3 mmol/L (0.5 – 2.0 mmol/L). Serum glucose was 277 mg/dL. CT Chest demonstrated a left lower lobe consolidation with multiple, loculated pleural fluid collections. CT Abdomen was negative for intra-abdominal infection. Transesophageal echocardiography was negative for vegetations. A chest tube was placed to drain the largest left loculated pleural effusion. Blood, sputum and pleural fluid cultures grew Salmonella Enteritidis, consistent with pneumonia complicated by empyema. The patient was initially treated with vancomycin, metronidazole, ceftriaxone and azithromycin and narrowed to ceftriaxone per susceptibilities. He underwent successful thoracic decortication of the empyema and completed 5 weeks of ceftriaxone post-procedure with resolution of symptoms.
Discussion: This case illustrates an adult with systemic, nontyphoid Salmonella infection complicated by pneumonia and empyema and the lack of a preceding GI illness. Salmonella infection is classified into typhoid and nontyphoid (NTS) subtypes. Infection with NTS is typically a self-limited gastroenteritis resulting from fecal-oral transmission from contaminated water and food. Approximately 1.2 million cases and 450 deaths are attributed each year to NTS in the United States. About 5% of infections progress to bacteremia, which can lead to extraintestinal focal infections (EFIs) including endarteritis, septic arthritis, osteomyelitis, and pneumonia/empyema–especially in immunocompromised hosts. Additional risk factors for EFIs include age greater than 60, diabetes mellitus, hypertension and chronic lung disease. Long-standing diabetes is thought to increase the risk for NTS infection through reduced gastric acidity and impaired gut motility from associated enteric neuropathy. Initial management involves parenteral antibiotic therapy against Gram negative enteric bacteria and source control of any focal infections. Prompt recognition of uncontrolled diabetes mellitus as a risk factor for complicated NTS infection and improving glycemic control in these patients may be critical to effective management for this high-risk population.
Conclusions: Salmonella bacteremia with pneumonia and empyema is a rare manifestation of nontyphoid Salmonella infection, and can present without GI symptoms. Treatment involves prompt initiation of parenteral antibiotic therapy and achieving adequate source control of the infection. Further, it is critical to recognize uncontrolled diabetes mellitus as a predisposing risk factor for systemic nontyphoid Salmonella infection, with or without extraintestinal manifestations.