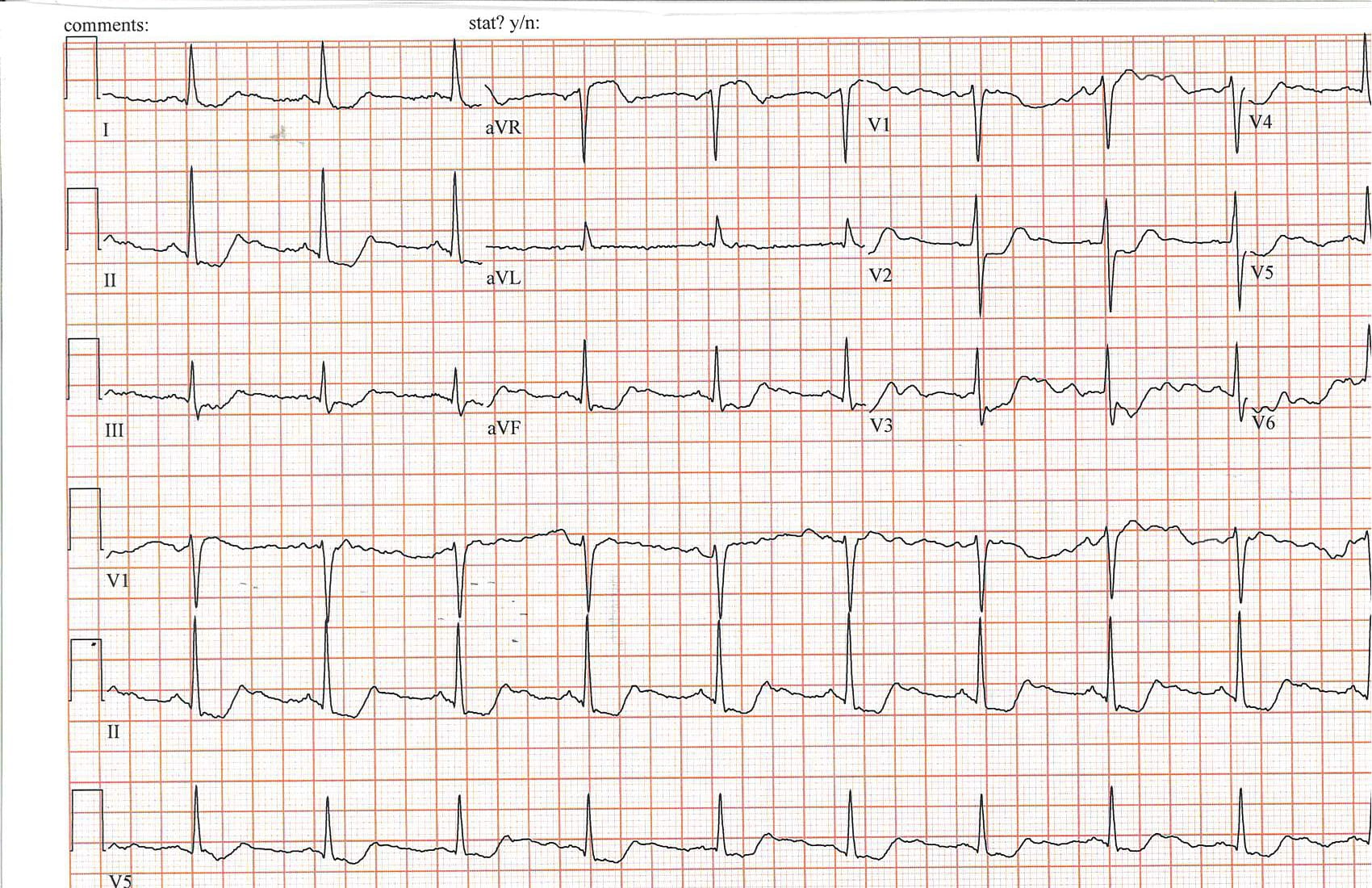
Case Presentation: A 69-year-old female presented to the Emergency Department with progressive weakness, nausea, vomiting, diarrhea, abdominal pain, and confusion for several weeks following an eye surgery the month prior, with symptoms acutely worsening over the last week. On the day of admission, she was found disoriented and clinging to a doorway at home, unable to move her legs with arms contracted to her chest. Her past medical history includes Grave’s disease, primary hyperparathyroidism, Celiac disease, Renal Cell Carcinoma, hypertension, and gastroesophageal reflux disease on proton pump inhibitor (PPI). On physical exam she was tachypneic and generally uncomfortable, with diffuse abdominal tenderness, dry mucous membranes, and positive Chvostek sign. She was alert and oriented but with poor recall of recent events and psychomotor agitation. Laboratory tests were significant for an undetectable magnesium level with associated hypocalcemia, hypokalemia, hypophosphatemia. Troponin and lactate levels were elevated. Thyroid function tests and creatinine were normal. An EKG showed diffuse ST depression in inferior and anterior leads, ST elevation in V1, and normal intervals. CT imaging of head, chest, abdomen, and pelvis was unremarkable. She was admitted to the hospital for non-ST elevation myocardial infarction (NSTEMI) in setting of significant electrolyte derangements. Aggressive electrolyte replacement was initiated with volume resuscitation. PPI was discontinued. A heparin drip was started, but EKG abnormalities and troponin levels normalized with electrolyte replacement and a stress echocardiogram was negative for ischemia. A fractional excretion of magnesium was elevated, but obtained after magnesium replacement had been initiated. Full electrolyte stabilization and complete return to normal mental status took several days of aggressive replacement and patient was eventually discharged on oral magnesium supplementation.
Discussion: Magnesium is important in many key functions of the body. It is required for all enzymatic reactions that utilize ATP and is involved in movement of other electrolytes across cell membranes. The vast majority of magnesium is stored in bone, with proportionally very little able to be measured in the serum. Loss of magnesium can occur in several ways, including malabsorption, gastrointestinal losses, medication effects, and renal wasting. The earliest manifestations of hypomagnesemia are often neuromuscular and neuropsychiatric. Life threatening effects include tetany, coma, cardiac arrhythmias and, less commonly, cardiac ischemia, often as a direct result of magnesium’s effect on potassium and calcium homeostasis. In this patient, chronic hypomagnesemia due to long-term PPI use and possible malabsorption in celiac disease was worsened by outpatient discontinuation of oral magnesium replacement shortly before eye surgery. Post operative nausea and vomiting then led to an electrolyte crisis with extended recovery likely due to depletion of total body magnesium.
Conclusions: Severe hypomagnesemia is a life threatening condition characterized by abnormal neurologic and neuromuscular activity as well as cardiac effects ranging from arrhythmias to ischemia. Recovery can be prolonged when body stores are severely depleted. It is important for those who are prone to hypomagnesemia, especially the elderly, those on PPIs, and those at risk for malabsorption to ensure adequate intake either through diet or supplementation.