Background: Many hospitalized patients spend most of their admission laying in their hospital beds. This can lead to in-hospital complications such as skeletal muscle atrophy, bedsores, and venous thromboembolism. In-hospital decline in ability to perform ADLs is associated with need for post-acute facility placement and readmission. We aimed to increase the percentage of patients admitted to a general medicine inpatient service who met their goal Johns Hopkins Level of Mobility (JH-LM) twice per day from 0% to 75%, over a 9-month period in 2019.
Methods: A multidisciplinary mobility team was formed. The team used QI methodology, with multiple ramps of iterative PDSA cycles, to approach the problem. We began by educating patient care technicians (PCTs) and nurses (RNs) on the floor about how to safely mobilize patients, as well as how to use the JH-LM (a validated system of describing patients’ mobility) to assess a patient’s mobility goals. We instituted a multidisciplinary “mobility rounds” each weekday at 8:30 AM, which was attended by the inpatient hospitalist attending, the nurse clinician, the case manager, the physical therapist, and each patient’s bedside nurse. During these 15-minute rounds, the team would discuss each patient’s mobility, assign them a goal JH-LM, and fill out a bedside placard which listed the patient’s goal JH-LM and what level of assistance they required to safely achieve this goal. Staff manually recorded what JH-LM was achieved when a patient was mobilized, and this data were followed daily. Staff received feedback bi-weekly about what percentage of patients on the unit were meeting their goal JH-LM twice daily. Information sheets about mobility were also created and distributed to patients with higher baseline levels of mobility to engage them in their own mobility. RN, PCT, and physician attitudes about mobility and communication on the unit were surveyed before and after the project using the Johns Hopkins Patient Mobilization Survey. Falls, Length of stay, and readmissions were followed monthly as balancing measures.
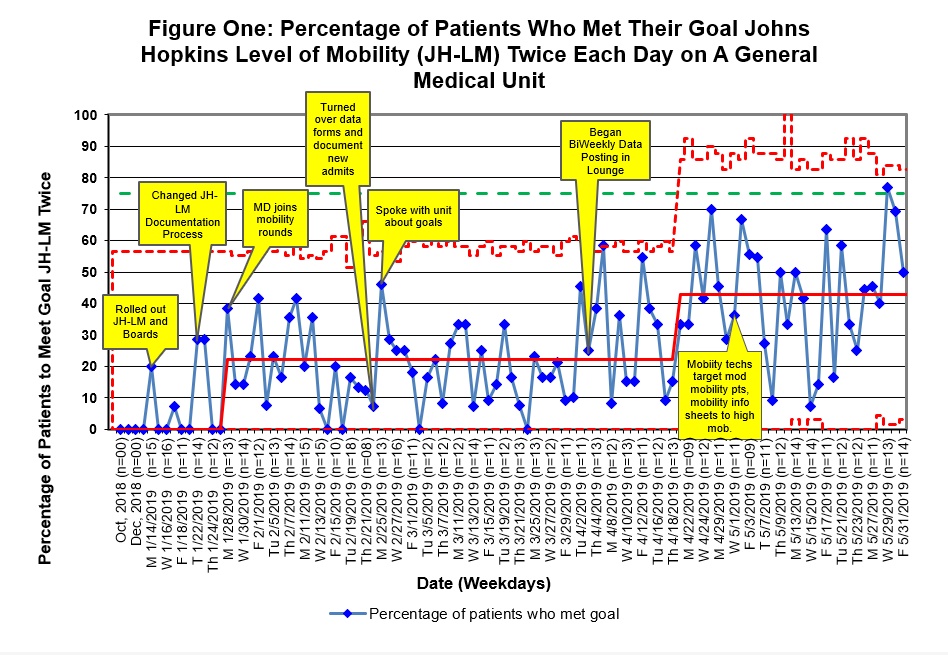
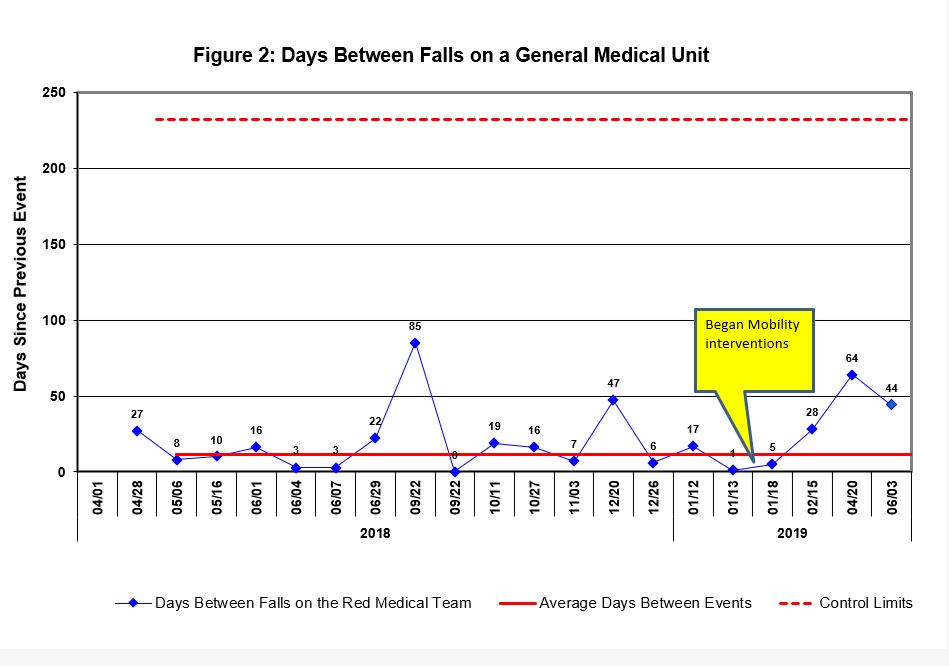
Results: We succeeded in increasing the average percentage of patients who reached their goal JH-LM level from 0% at the start of the project to 44% by the project’s conclusion, with several instance of special cause variation related to our interventions (Figure 1). By the end of our intervention period there were several days where we achieved our goal of 75% of patients reaching their JH-LM goal mobility twice. There was no increase in falls on the unit during the time of the intervention- in fact there was a trend towards increased days between falls (Figure 2). There was no special cause variation in length of stay or readmissions. Physician, nurse, and PCT attitudes about mobility and communication on the unit showed improvements.
Conclusions: Our multidisciplinary approach to improving mobility was successful in improving our patients’ mobility, although we did not reach our goal. Our goal may have been unrealistic due to a lack of clear best practices/benchmarking for mobility. We did not see an increase in falls during our intervention period. All members of the multidisciplinary team showed improved attitudes about patient mobility and the communication of the interdisciplinary team and found the project to be a valuable use of their time. We are planning to continue mobility rounds and bedside mobility goal placards, while spreading the intervention to the other general medical team which is housed on the unit.