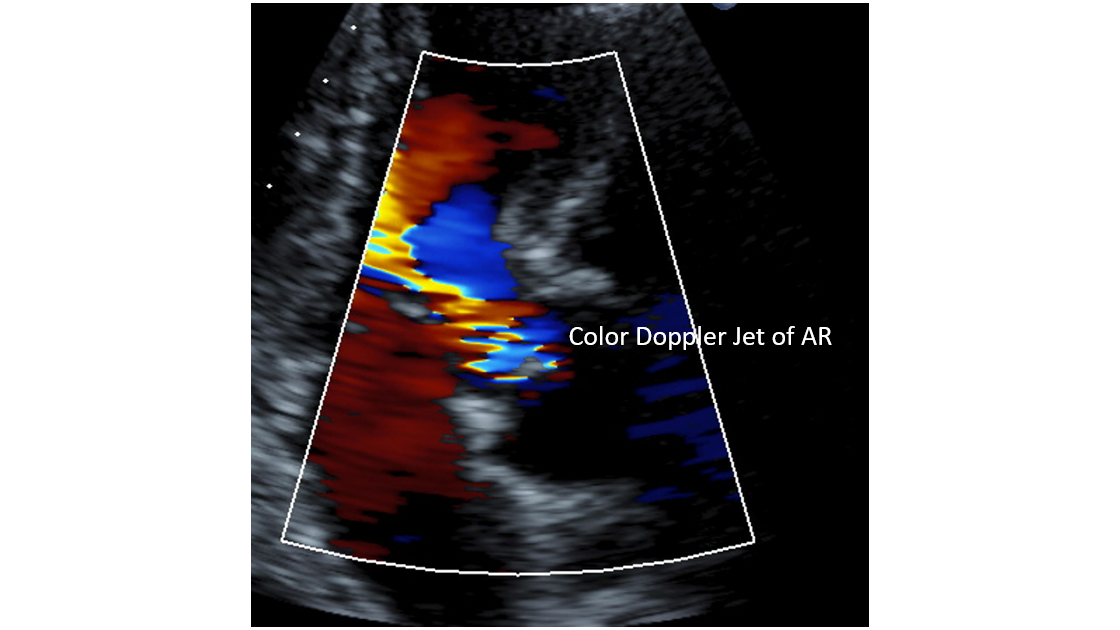
Case Presentation: A 57-year-old man with history of Stage IV pancreatic adenocarcinoma, coronary artery disease, and deep venous thrombosis presented to the emergency room with chest pain and acute bilateral lower extremity swelling. The chest pain began several hours prior to admission and the swelling developed over the past 3 days. On exam, he had a new grade 2 systolic murmur and 1+ edema to his bilateral lower extremities. Troponins were negative. CT pulmonary embolism study found an acute pulmonary embolism in the left and right lower lobe pulmonary arteries. Ultrasound of the legs revealed thrombosis in the bilateral femoral veins. The patient was started on heparin drip. Echocardiogram revealed an EF of 68%, with a new large mobile density on the aortic valve consistent with a vegetation. Antibiotics were started but blood cultures and workup for infectious endocarditis remained negative. The patient was diagnosed with nonbacterial endocarditis. MRI brain and TEE, which are usual next steps, were discussed but deferred by the patient due to interest in hospice enrollment.
Discussion: Marantic endocarditis (ME) is characterized by a sterile vegetation on a cardiac valve (most commonly aortic and mitral). The deposits formed on the heart valve are made of fibrin and platelets (5). It can be associated with auto-immune conditions, hypercoagulable states, trauma, and malignancy (2). It is a rare entity with unknown exact prevalence but is an important diagnosis for hospitalists to consider because of significant therapeutic implications. In one study performed in Europe, they found 47 cases over a ten-year time period (1). Over the past decade, with increased access and advancement in echocardiography, there has been a significant increase in the number of cases reported (5).ME is a distinct entity from bacterial endocarditis, usually recognized with identification of a valvular vegetation with negative blood cultures. ME can be a presenting feature of paraneoplastic hypercoagulability and should prompt further work-up for underlying malignancy. Lung and pancreatic cancer are the most common associated sites of cancer (2). Acute embolic stroke is a presenting feature in about half of patients with this condition (2,5). Importantly, in cancer patients, ME is indicative of an advanced stage of illness, associated with increased risk of in-hospital and one-year mortality, around 55% (6). Thus, diagnosis of ME in patients with malignancy should prompt hospitalists to initiate goals of care discussions with patients. Generally, treatment consists of addressing the underlying malignancy and anticoagulation (4). Surgery may have a role, depending on the clinical severity of the presentation and the patient’s prognosis and goals of care. Misdiagnosis of ME as bacterial endocarditis can lead to unnecessary antibiotics and potentially delay appropriate therapy for the underlying condition.
Conclusions: Hospitalists should be vigilant about considering marantic endocarditis in patients with cancer or autoimmune conditions, especially if they are presenting with a new heart murmur and/or embolic phenomena (stroke, DVT, PE, organ or limb infarction). Treatment of ME in cancer patients consists of addressing the underlying malignancy and initiation of anticoagulation. ME represents an advanced stage of illness and should prompt advance care planning. If diagnosed and treated early by hospitalists, then it may prevent significant morbidity in patients.