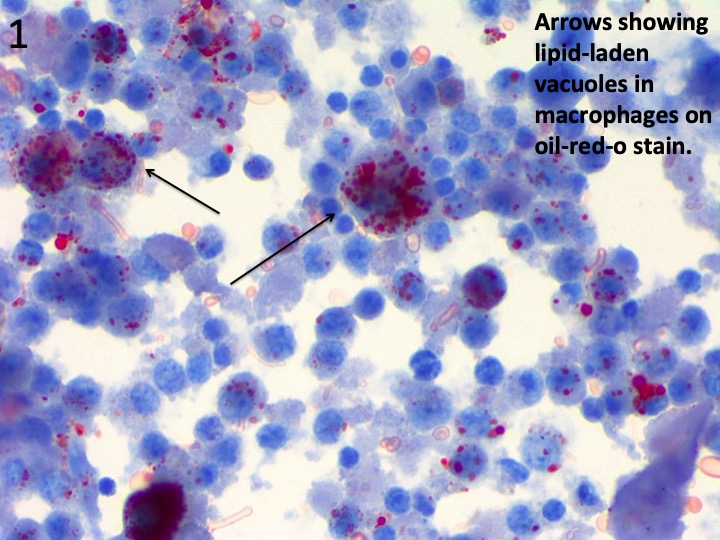
Case Presentation: A 24-year-old male presented to the hospital with abdominal pain, vomiting, and fevers for one week, followed by dyspnea and cough. He denied animal exposure or recent travel, but admitted to vaping daily and using marijuana occasionally. On admission, vital signs were as follows: temperature 101 F, BP 107/64 mmHg, heart rate 109 bpm, respiratory rate 17, saturating 98% on room air. Physical examination was unremarkable, and demonstrated clear lungs and a soft non-tender abdomen. Laboratory results were significant for: white blood cells 14.9 k/uL with 93% polymorphonuclear cells, platelet count 313 k/uL, normal electrolytes, ALT 306 U/L, AST 167 U/L, alkaline phosphatase 68 U/L, total bilirubin 0.7 mg/dL, lipase 15 U/L, lactic acid 2 mmol/L, C-reactive protein 29.18 mg/dL, erythrocyte sedimentation rate 106 mm/hr, and immunoglobulin E 169.5 IU/mL. Extensive infectious and autoimmune workup was negative. Urine toxicology was positive for cannabinoids. Computed tomography of the chest showed bibasilar groundglass opacities in the lungs. He was empirically managed with vancomycin and pipercillin-tazobactam. By Day 3, he continued to be febrile and became increasingly hypoxemic. A chest X-ray revealed worsening bibasilar infiltrates prompting bronchoscopy. Bronchoalveolar lavage demonstrated intracytoplasmic lipid-laden vacuoles in >50% of alveolar macrophages by oil-red-O stain (Figure 1). Acid-fast stains, fungal, and bacterial cultures were negative. He was then started on intravenous methylprednisolone. His fevers and hypoxemia resolved and liver enzymes normalized and thus antibiotics were discontinued. He was discharged on Day 7 with an oral prednisone taper.
Discussion: The pathogenesis of vaping-induced lung injury has not been clearly delineated as yet. Most reported cases highlight airway-centric non-granulomatous inflammatory lung disease or diffuse alveolar damage. Although macrophages show lipid-laden vacuoles, radiologic findings typical for exogenous lipoid pneumonia are not seen due to inflammatory changes probably masking the radiolucent changes related to exogenous lipoid pneumonia. However, the relatively non-specific finding of lipid laden macrophages as a marker of alveolar inflammation in the right clinical setting should increase suspicion of vaping-induced lung injury and aid in the expedited use of steroids early in the course of the disease.
Conclusions: The emergence of “vaping” – the process of inhaling aerosols created by heating a liquid containing substances such as nicotine or cannabinoids mixed with additives like glycerol, propylene glycol, and vitamin E – has led to an increased incidence of acute and sub-acute lung injury, particularly in young adults. Given the novelty of this disease process, specific pathogenesis remains uncertain. In combination with lack of specific diagnostic testing, vaping-induced lung injury poses a diagnostic challenge. Bronchiolar lavage findings consistent with alveolar inflammation combined with pertinent history of vaping should trigger clinical suspicion and timely administration of glucocorticoid therapy. Swift initiation of proper treatment is imperative to achieve favorable outcomes in this patient population.