Background: Half of US hospitalists have contracts with pay-for-performance incentives based on quality outcomes such as length of stay (LOS) and readmission according to the 2023 State of Hospital Medicine Report. Traditionally, these measures have been linked to the discharging provider. However, as the length of a patient’s stay increases, the influence of the discharging provider over metrics such as LOS and readmission decreases. This standard attribution model, which links outcomes from prolonged and complex cases solely to the discharging provider, has led hospitalists to mistrust their quality metrics. Our study aims to define and evaluate a more equitable attribution model for assigning LOS and readmission to a provider with genuine influence over these outcomes, thus improving trust and engagement with these metrics.
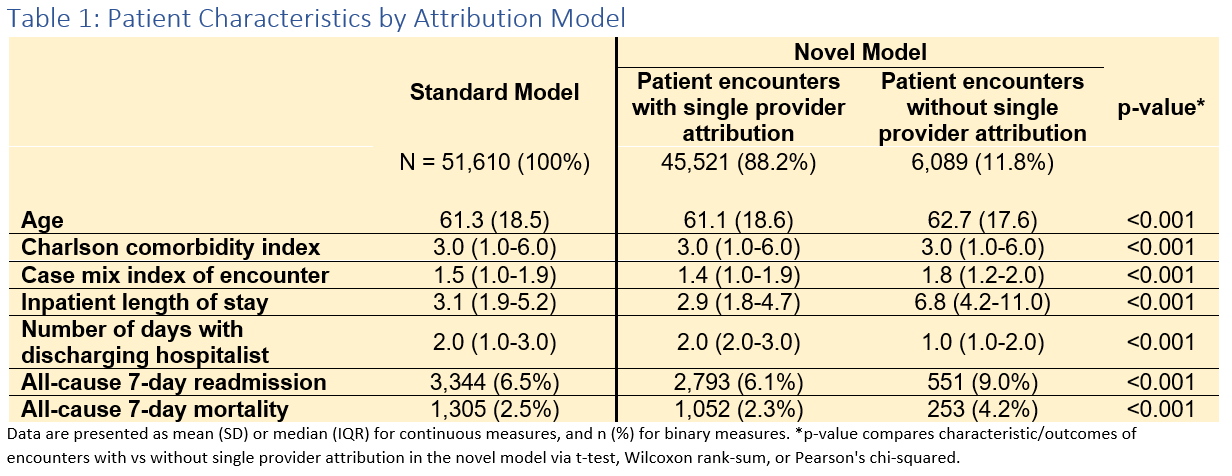
Methods: Our novel model assigns LOS and readmission to a single provider only if that provider oversees at least 30% of the inpatient duration and discharges the patient, while all encounters continue to have group level attribution by hospital. This is the first attribution model reported that does not stipulate that all patient encounters have a single provider assigned to these quality metrics, recognizing the team approach required for the care of extended inpatient stays. We compared our model to the standard model across three years of data at 5 Intermountain Health hospitals capturing 51,610 encounters and 130 providers meeting encounter thresholds for assessment in the analysis. Quality metrics from the novel model are compared to standard model by top/bottom-half concordance and average change in rank by provider. We then report the encounter characteristics of those patients newly excluded from single provider outcomes attribution.
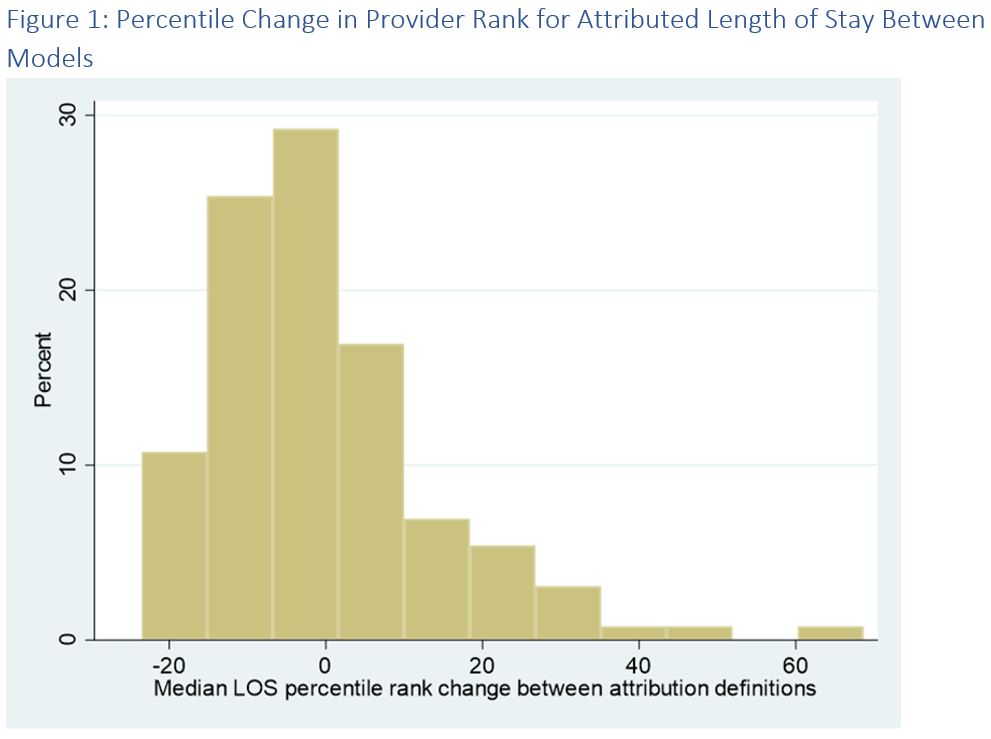
Results: Top-half/bottom-half concordance between the novel model and the standard model is 84.6% (indicating 15.4% of providers in the top or bottom-half of one model are not in the same half of the other). Our novel model excludes 11.8% of inpatient encounters from single provider attribution, while all encounters continue to have group level attribution by hospital. The LOS percentile rank for the average provider changes 10.2% (SD 10.0%) within hospital group between models and one provider increased their rank by 69% (35 places) (Figure 1). In the novel model, median (IQR) LOS and median encounter days with discharging provider was 2.9 days (1.8-4.7) and 2.0 days (2.0-3.0) for patients continuing to have single provider attribution vs 6.8 days (4.2-11.0) and 1.0 day (1.0-2.0) for encounters no longer having single provider attribution (Table 1). For those encounters no longer meeting single provider attribution in the novel model, readmission rates were 48% higher and mortality rates 83% higher.
Conclusions: Our model significantly improves the influence of providers over the encounter outcomes by which they are measured, while excluding only 11.8% of encounters from single provider attribution. We believe that moving quality metrics to our model will improve provider faith in the attributed metrics and engagement with data-driven quality improvement.