Background: The direct oral anticoagulants (DOACs) apixaban and rivaroxaban are increasingly prescribed due to convenient oral formulation without the need for routine laboratory monitoring and are now commonly regarded as first line anticoagulants in most cases of venous thromboembolism (VTE). However, the optimal choice of subsequent anticoagulant in instances of first line DOAC failure is unclear. Our goal is to describe and compare outcomes with second line anticoagulants used after failure of first line DOACs.
Methods: Patients seen at our urban tertiary care hospital system for an episode of acute VTE between 1/1/2010 and 9/1/2022 initially treated with either apixaban or rivaroxaban who experienced a subsequent recurrent thrombosis while on anticoagulation (1st recurrent thrombosis) were included. Patients on DOAC therapy for less than two weeks were excluded. Clinical demographics, therapy, and outcomes were extracted by manual chart review. Extracted clinical data included cause and location of initial and 1st recurrent thrombosis, 2nd (subsequent) anticoagulant therapy (warfarin vs dabigatran vs enoxaparin), duration of 2nd anticoagulant therapy, and cause for 2nd anticoagulation cessation. Extracted outcomes included incidence of major bleeding, rate of 2nd recurrent thrombosis (i.e., failure of 2nd anticoagulant), and death from any cause. Distributions of continuous and categorical variables were compared using analysis of variance (ANOVA) and chi-square test, respectively. Risk for 2nd recurrent thrombosis was determined by a multivariable Cox adjusting for anticoagulant type, etiology of 1st recurrent thrombosis, and location of 1st recurrent thrombosis. Time to 2nd recurrent thrombosis was compared between anticoagulant groups by the Kaplan-Meier test.
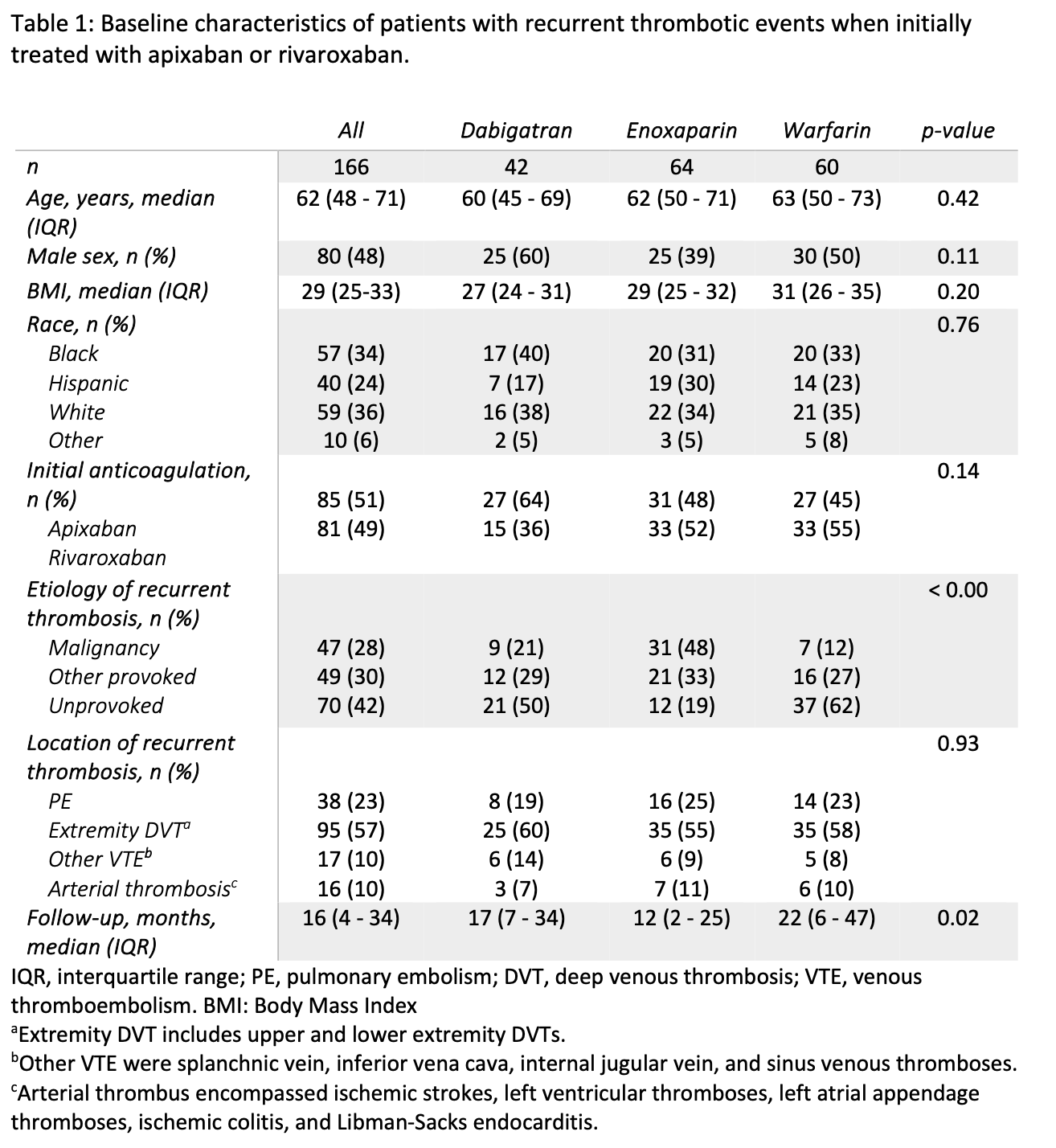
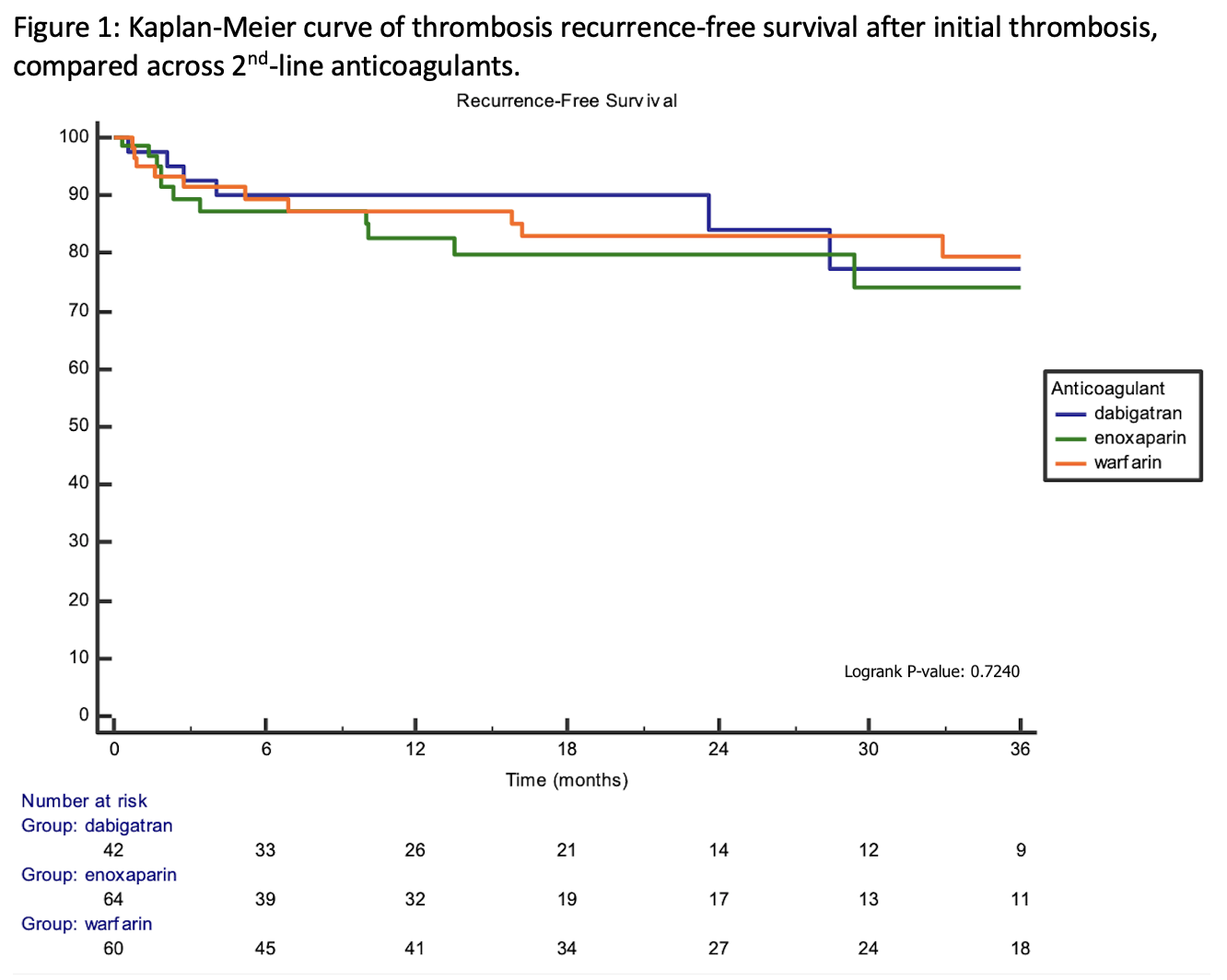
Results: In total, 166 patients treated with warfarin, dabigatran, or enoxaparin after antecedent apixaban or rivaroxaban failure (1st recurrent thrombosis) were included (Table 1). 51% and 49% of patients failed apixaban and rivaroxaban respectively. Following apixaban or rivaroxaban failure (1st recurrent thrombosis), the subsequently prescribed anticoagulant was warfarin in 60 patients (36%), dabigatran in 42 patients (25%), and enoxaparin in 64 patients (39%). Enoxaparin was preferentially prescribed in patients with a malignancy-associated etiology for 1st recurrent thrombosis (p < 0.01). The median follow-up time in our cohort was 16 months (interquartile range 4-34 months). There was no difference in 2nd recurrent thrombosis-free survival among patients treated with dabigatran, warfarin, or enoxaparin (p=0.72; Figure 1). In a multivariable Cox model adjusted for etiology and location of 1st recurrent thrombosis, dabigatran (HR 0.86, p = 0.8) and warfarin (HR 0.90, p = 0.8) were not superior to enoxaparin. There was also no difference in risk for major bleeding events (p=0.30).
Conclusions: In this large retrospective analysis of patients failing first line DOAC therapy, rates of 2nd recurrent thrombosis and bleeding did not differ between subsequently chosen anticoagulants. Our study provides further evidence that the optimal 2nd anticoagulant is not clear, and the choice of 2nd anticoagulant should continue to balance patient preference, cost, and provider experience.