Background: The Association of American Medical Colleges identifies consideration of social determinants of health (SDoH) and patient-specific factors as key components of entrustable professional activities (Englander 2016). Prior studies of medical students and Internal Medicine (IM) residents demonstrated baseline gaps in integrating SDoH into clinical reasoning (CR) in the outpatient setting (Schwartz 2010, Wilhite 2020), highlighting the need for further inpatient research. This is particularly time-sensitive, as the Centers for Medicare & Medicaid Services (CMS) will require screening for social needs in all adult inpatient encounters starting in January 2024 (CMS 2023).
Purpose: We designed and implemented a longitudinal curriculum within the IM clerkship to teach clinical medical students to incorporate SDoH into CR through the use of contextual problem representations. We will prospectively assess the impact of this curriculum on performance in a novel SDoH-focused standardized patient (SP) encounter and retrospectively compare write-up content in a final graded SP encounter to historical controls. This study has been approved by the Institutional Review Board.
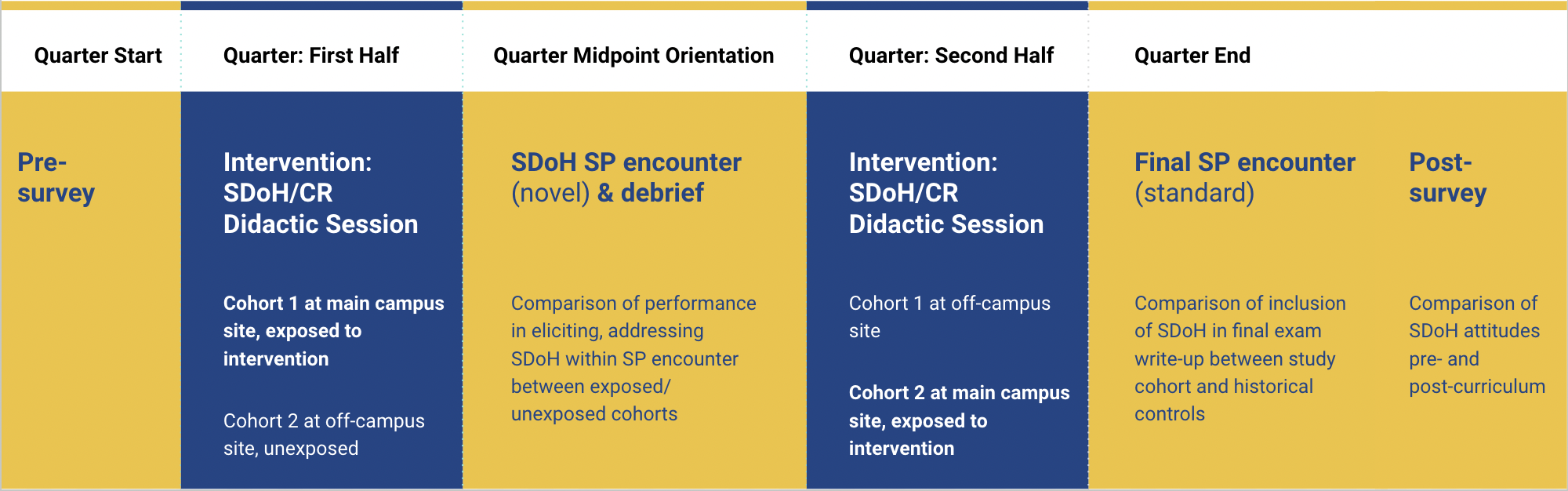
Description: The curriculum was implemented during the IM clerkship starting in August 2023. The clerkship consists of two 4-week inpatient site rotations, a midpoint orientation with a formative SP encounter, and a final graded SP exam. All students rotate through the main campus inpatient site during either the first or second half of the clerkship. The curriculum includes (Figure 1):1) Intervention: Case-based didactic session during the students’ main campus rotation. Students are taught to apply a contextual problem representation to improve clinical reasoning using 2 cases.2) Assessment: Midpoint SP encounter, a novel case describing a patient with acute decompensated heart failure triggered by multiple SDoH needs. Students also participate in a debrief reemphasizing the use of the contextual problem representation.We are primarily performing a prospective posttest only quasi-randomized control educational trial. Students will be assessed by their performance in the midpoint SP encounter, specifically performance in eliciting SDoH and integrating SDoH into their assessment and plan. This will be assessed using checklists completed by SPs and independent blinded coding of the student write-ups. Students are quasi-randomized by rotation site to participate in the didactics either in the first half (exposed group) or the second half (unexposed group). We will secondarily perform a retrospective analysis comparing SDoH content in a final graded SP encounter write-up between students in the 2021-2022 academic year (pre-curriculum) and students in the current academic year (post-curriculum). We will also assess change in student attitude, knowledge, and experience surrounding CR, SDoH, and the curriculum with a pre- and post-clerkship survey.
Conclusions: We successfully implemented the curriculum and curricular assessment with completion of data collection planned for July 2024. Preliminary survey data from three clerkship quarters will be available for dissemination by April 2024. Our findings will help to better characterize best practices for teaching undergraduate learners to integrate SDoH into CR.