Background: Previous research describes different models for mentorship of new hospitalists, however, most of these models are geared towards development in research, education or quality improvement skills. There is scarce work describing programs promoting the clinical development of new hospitalists. New hospitalists may face cases that are complex due to clinical, social, or administrative challenges and benefit from mentorship from more experienced hospitalists.
Purpose: To create a peer resource for hospitalists to discuss challenging or complex patients and promote clinical development at our large urban academic medical center.
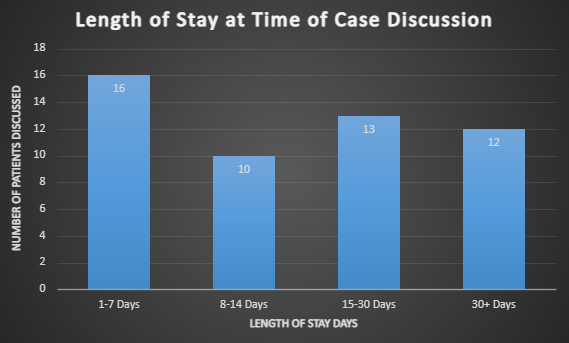
Description: A needs assessment survey was administered to 40 full-time hospitalists with 32 respondents who completed the survey. There was a spread of experience with 10 respondents with under 3 years of experience and 18 respondents with more than 5 years of experience. Respondents indicated that they would want an additional resource to discuss patients with complex psychosocial issues (81%), overcoming discharge barriers (69%), knowledge of inpatient resources (47%), and complex clinical decision making (47%). Most respondents (88%) reported discussing challenging cases informally with peers. Respondents indicated that they would use such a mentoring resource weekly (10), monthly (9), or a few times a year (14); none said they would never use this resource. We implemented a peer mentoring model in which 3 senior hospitalists (SHs) with at least 10 years of clinical experience and administrative leadership experience were available to discuss complex cases. The SHs were available to discuss cases on a weekly 30-minute period through a video conferencing platform (though this was later changed to a shorter daily schedule on weekdays) and also through a group email.From implementation in February through October, 58 cases were discussed with the SHs for an average of 6.4 cases per month. Most of the cases escalated were for assistance in addressing discharge barriers (16), resource utilization (14), clinical decision-making (12), and patient or family conflict (5). More than half the cases (30) were escalated by hospitalists with 3 years or less of experience. There was an almost equal number of patients discussed on resident teaching teams (26) and primary attending teams (22). Thus far, 51 cases were reviewed for quality outcomes, demonstrating an average length of stay (LOS) of 26 days, median LOS of 14 days and 5 cases in which the LOS was more than 90 days. There were 9 deaths among these 51 patients for a mortality rate of 17.6%. During this same period, the overall mortality for patients in the hospitalist service was 2.7%.
Conclusions: A peer mentoring model for clinical cases can be a helpful and frequently utilized resource for hospitalists. While many hospitalists reported informally discussing challenging cases with peers, we found regular use of the SHs to discuss challenging cases after implementation. Hospitalists of all years escalated cases, though most cases were brought by hospitalists with less than 3 years of experience. The patients discussed had long length of stay and were sick, with higher mortality rates than our average patient.