Case Presentation:
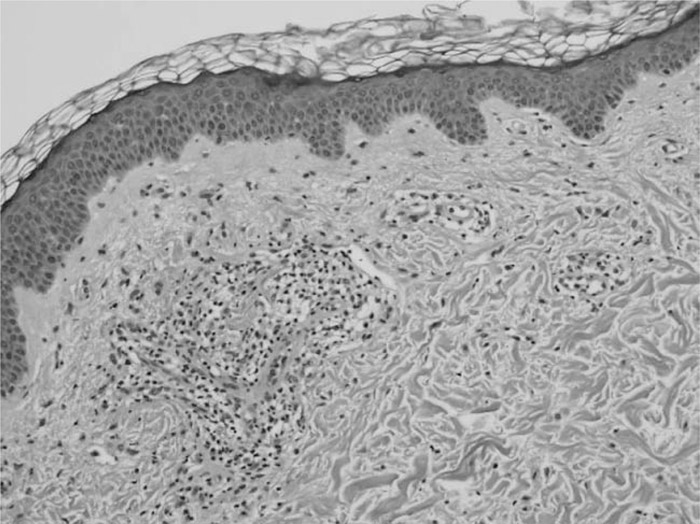
This is a 51‐year‐old woman with a medical history significant for a seizure disorder diagnosed after she had a tonic‐clonic type seizure at age 16. She was treated with phenytoin, but this was complicated by a rash at age 21. The patient was then managed with carbamazepine and was seizure free until age 50, when a seizure prompted a switch to lamotrigine. One month after achieving the full dose, the patient developed a rash with headache, fevers, and chills. When these symptoms persisted, the patient presented to the emergency department. Physical exam was notable for a temperature of 101.2°F, facial edema, and a rash of morbilliform erythematous papules and forming plaques, involving the trunk, arms, and legs but sparing the palms and soles. Laboratory data were notable for an ALT of 138 U/L, AST of 111 U/L, alkaline phosphatase of 910 U/L, and white blood cell count of 8.4 × 103 cells/mL3, with 6% eosinophils. Pathology was notable for a mixed infiltrate consistent with a drug eruption. The patient was treated successfully with corticosteroids and the discontinuation of lamotrigine. When she became afebrile and her liver function tests began to trend down, she was transferred to the neurology service. There she was transitioned to levetiracetam. She denies seizures and reports improvement of her rash, but with some residual hyperpigmentation.
Discussion:
Drug rash with eosinophilia and systemic symptoms (DRESS) syndrome is a rare but serious adverse drug reaction estimated to occur at a rate 0.01% to 0.1% in patients treated with antiepileptic drugs. To make a diagnosis, the patient must have skin, blood, and systemic involvement. Mucocutaneous features include facial edema and/or morbilliform eruption. Hematologic features include eosinophilia and/or atypical lymphocytes. Systemic features may include lymphadenopathy, hepatitis, nephritis, pneumonitis, or carditis. Once the diagnosis is made, the mainstay of therapy is removing the offending medication. Debate is ongoing about whether steroids are indicated because of a lack of clinical trials; currently, they are used when there is systemic involvement and tapered slowly.
Conclusions:
Although these medications are often prescribed by neurologists, patients with these symptoms will likely present to medical hospitalist services because of the presence of systemic symptoms and laboratory abnormalities.
Disclosures:
A. E. Cohen ‐ none; K. Hochman ‐ none