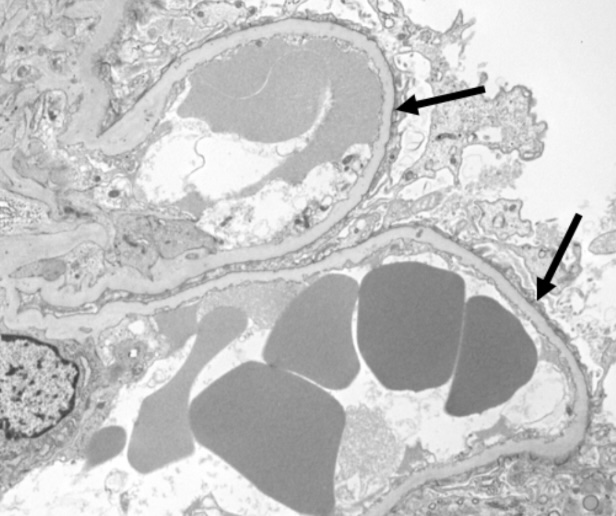
Case Presentation: This patient is a 53-year-old male with type 1 diabetes, hyperlipidemia and hypertension who presented with a 5 week history of diffuse whole body edema and an unintentional weight gain of 10 kilograms. He was started on bumetanide, losartan and empagliflozin by his outpatient team with brief improvement but subsequently worsened. He presented to the emergency department with these symptoms as well as decreased urine output and was found to have anasarca with evidence of nephrotic syndrome. Urinalysis was notable for a 24-hour protein of 9.75 grams. Serum labs were notable for creatinine of 2.5 mg/dL (baseline 1.4-1.6), albumin 1.9 g/dL, IgM 3.67 g/dL. Serum protein electrophoresis revealed IgM spike at 3.0 g/dL and elevated IgM. Renal ultrasound, right upper quadrant ultrasound and echocardiography were unremarkable. A kidney biopsy revealed glomerular disease consistent with nephrotic syndrome. Bone marrow biopsy revealed lymphoid aggregates and clonal proliferation consistent with both chronic lymphocytic leukemia (CLL) and Waldenstrom’s macroglobulinemia (WM) which, to our knowledge, is the first case where CLL and WM present simultaneously and with nephrotic syndrome as the presenting syndrome . The patient was treated with steroids as well as a rituximab-based chemotherapy regimen. He was discharged with zanubrutinib and torsemide, and he is currently at his baseline creatinine (1.5 mg/dL) and is no longer on zanubrutinib.
Discussion: Fluid overload comes with a broad differential; a thorough workup is required to pinpoint the etiology. Glomerular disease, although rare, can present with gradually or rapidly progressing symptoms. Although many cases of nephrotic syndrome are idiopathic, many occur secondary to an underlying disease, such as HIV, Hepatitis B, solid tumors or hematologic malignancy. CLL and WM are two hematologic malignancies that often present without symptoms, but in some cases they can present solely with renal manifestations.Although it can be difficult to elucidate a causal relationship between these malignancies and minimal change disease, their association warrants a thorough workup. They should be on the differential for any patient presenting to a hospital or emergency department setting with nephrotic syndrome of unknown etiology.
Conclusions: Chronic lymphocytic leukemia (CLL) and Waldenstrom’s macroglobulinemia (WM) have been shown in the literature to have renal manifestations. A rare presentation of both conditions can be kidney disease, specifically glomerular. This case highlights the importance of recognizing nephrotic syndrome as a potential initial presentation of hematologic malignancy. The diagnosis of minimal change disease in an adult patient with underlying CLL and WM emphasizes the importance of a comprehensive evaluation of nephrotic syndrome of unknown etiology. Early identification and treatment can significantly impact patient management and improve patient outcomes.