Case Presentation:
A 29-year-old female presented with right femoral fracture after twisting her leg. One month prior she saw orthopedic surgery for foot pain. She was referred to endocrinology after DEXA scan showed severe osteoporosis with T score of -4.1. She also had elevated calcium and parathyroid hormone (PTH) and undetectable Vitamin D levels. Sestamibi scan showed right lower pole parathyroid adenoma. She was diagnosed with primary hyperparathyroidism (PHPT) with severe vitamin D deficiency just prior to her admission and placed on Vitamin D replacement.
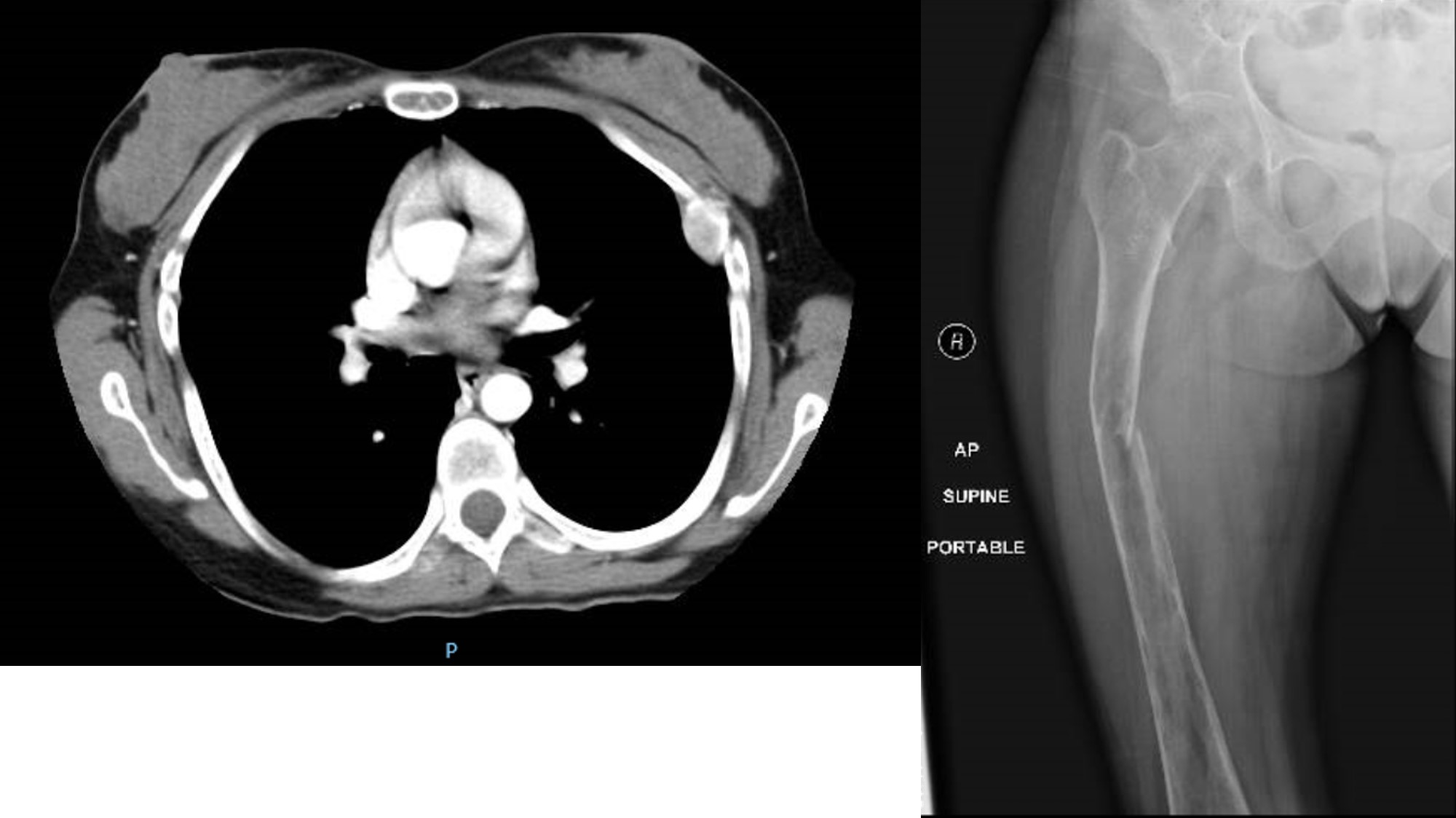
On admission, calcium was 14.1mg/dl, phosphorus 2.4mg/dl, magnesium1.9mg/dl, Vitamin D 15ng/ml, PTH 1463pg/ml, alkaline phosphatase 1534u/l and GFR 59. CBC was normal. X-ray showed pathologic fracture of the right femoral midshaft, severe osteopenia and multiple lytic intramedullary lesions with endosteal scalloping. Imaging of the left femur and bilateral tibia/fibula showed intramedullary and cortical lucencies consistent with brown tumors. CT chest demonstrated diffuse osteopenia with brown tumor on the left fourth rib. Three-phase bone scan revealed extensive increased radiotracer uptake involving the calvarium and appendicular and axial skeleton, representing diffuse metabolic disorder from hyperparathyroidism versus widespread osseous malignancy. The patient had internal fixation of the femur fracture and right parathyroidectomy. She was closely monitored for hungry bone syndrome and calcium, phosphorus and magnesium were repleted accordingly. She was treated with IV bisphosphonates and discharged home on oral calcium and Vitamin D. She was instructed to follow up with endocrinology and orthopedic surgery.
Discussion:
Clinical symptoms associated with hyperparathyroidism are weakness, fatigue, renal stones, fractures and osteitis fibrosa cystica (OFC). OFC is the classic skeletal manifestation of end stage PHPT characterized by skeletal demineralization, subperiosteal bone resorption, cortical thinning, pathologic fractures and brown tumors. Brown tumors are seen as expansile osteolytic lesions with osteopenia on plain radiographs and as well enhanced masses on CT. With routine laboratory screening, hypercalcemia due to hyperparathyroidism can be detected early; as a result, cases of OFC in developed countries are increasingly rare. Superimposition of vitamin D deficiency on PHPT may have a role in the development of these skeletal lesions. Treatment of OFC is surgical removal of the parathyroid adenomas. Bone lesions tend to recover spontaneously after correction of the PTH level, and surgical removal of OFC is usually unnecessary.
Conclusions:
OFC has become extremely rare in developing countries due to early detection of hypercalcemia and its subsequent treatment. However, awareness of this condition is important in the differential diagnosis of bony lesions that suggest malignant disease. Parathyroidectomy has been shown to result in the reversal of bone resorption and complete regression of brown tumors.