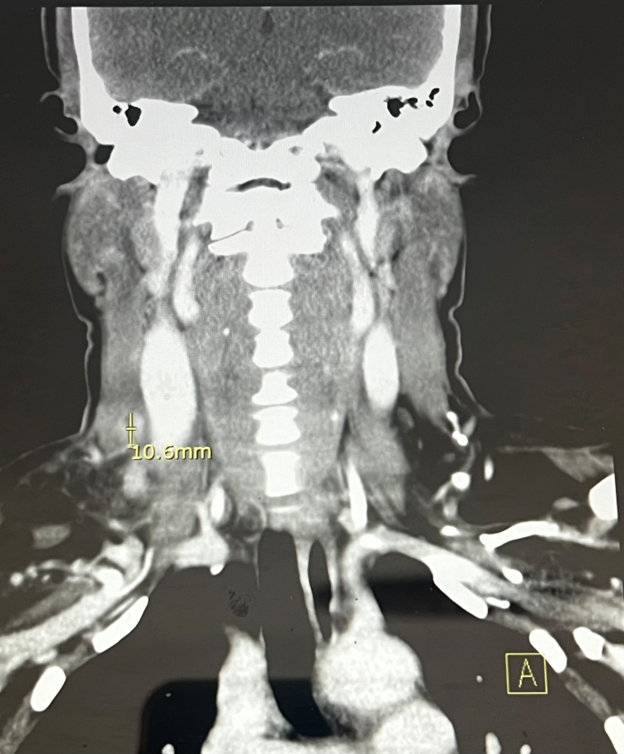
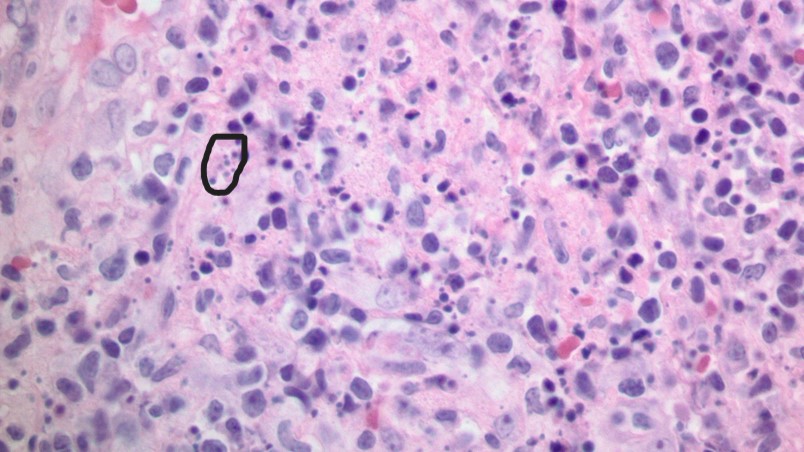
Case Presentation: A 37-year-old woman from Ghana presented to the hospital with a week duration of myalgias, right-sided neck pain, and right-sided neck swelling that she noticed three days before the admission. Physical examination was only positive for non-pulsatile, mobile swelling in the right anterior lower neck along the sternocleidomastoid. Labs were unremarkable, except for an erythrocyte sedimentation rate (ESR) of 47 and a C-reactive protein of 10.7. CT neck showed a conglomeration of mildly enlarged lymph nodes within the right anterior lower neck, with the largest being 1.3×1.4×1.1cm, with adjacent fat inflammation and myositis of the sternocleidomastoid muscle. No drainable collection was identified. Blood cultures were sent. The patient started on Unasyn at admission. CT chest and abdomen did not show any intrathoracic lymphadenopathy. Interventional radiology-guided lymph node biopsy and tissue pathology were consistent with classic histopathological characteristics of Kikuchi-Fujimoto lymphadenitis, with the presence of histiocytic necrotizing lymphadenitis with karyorrhectic debris, plasmacytoid dendritic cells and the absence of neutrophils. Antinuclear antibody (ANA), Human immune deficiency virus, Ebstein Barr Virus, streptococcus culture, thyroid, autoimmune, and respiratory viral panels were negative. Culture data from lymph node biopsy was negative for bacterial, mycobacterial, malignant, and fungal etiologies. The patient was discharged home. Six weeks of outpatient follow-up imaging showed a resolution of lymphadenitis.
Discussion: Kikuchi-Fujimoto Disease (KFD) is one of the rarest causes of lymphadenopathy in patients younger than 40. The disease is more prevalent in the Asian population due to HLA class II genes (Erbas et al., 2023). The cervical lymph node is involved in 60-90% of the cases, while axillary and supraclavicular involvement may also be seen in rare cases. Fatigue, fever, and myalgias are the common presenting symptoms. Common lab abnormalities include leukopenia, atypical lymphocytes, and ESR ( Masab et al., 2024). The cascade results in T cell-mediated apoptosis and the release of inflammatory cytokines. Excisional lymph node biopsy without neutrophils and eosinophils rules out infectious etiology (Masab et al., 2024). KFD is characterized by, 1. proliferative stage with follicular hyperplasia with histiocyte and lymphocytic infiltrates with the absence of neutrophils and eosinophils, 2. necrotizing stage with karyorrhexis and necrotic foci with intact lymph node architecture, and xanthomatous stage, with foamy histiocytes and regression of necrotic areas. Hematoxylin bodies are a marker for Systemic lupus erythematosus lymphadenitis (Masab et al., 2024). Patients with positive ANA are at risk for KFD recurrence (Baek, 2022). Immunohistochemistry differentiates from lymphomas and confirms KFD with positive staining for myeloperoxidase, CD68, lysozyme, CD163, and CD4, has CD 8 T cells and CD123 positive plasmacytoid dendritic cells (Masab et al, 2024). Most symptoms are resolved within one to four months. The recurrence rate is between 3% to 7% (Gism Elseed et al., 2022).
Conclusions: KFD is a rare, self-limiting cause of lymphadenopathy and fever of unknown origin. Effective care coordination between clinical teams and pathologists is vital for prompt diagnosis and treatment. Having a high index of suspicion is a crucial step in mitigating unwanted therapeutic approaches, reducing patient anxiety, and preventing misdiagnosis.